Within a large academic health system like UW Health, collaboration is an important element of our culture. It keeps the organization moving forward and allows staff and providers to share in both the work and rewards. When it comes to improvements, an identified gap or dissatisfier is followed by a plan for how to improve the issue. In these instances, frontline nurses are often the visionaries who ignite the change.
Improving post-hospital education for transplant patients
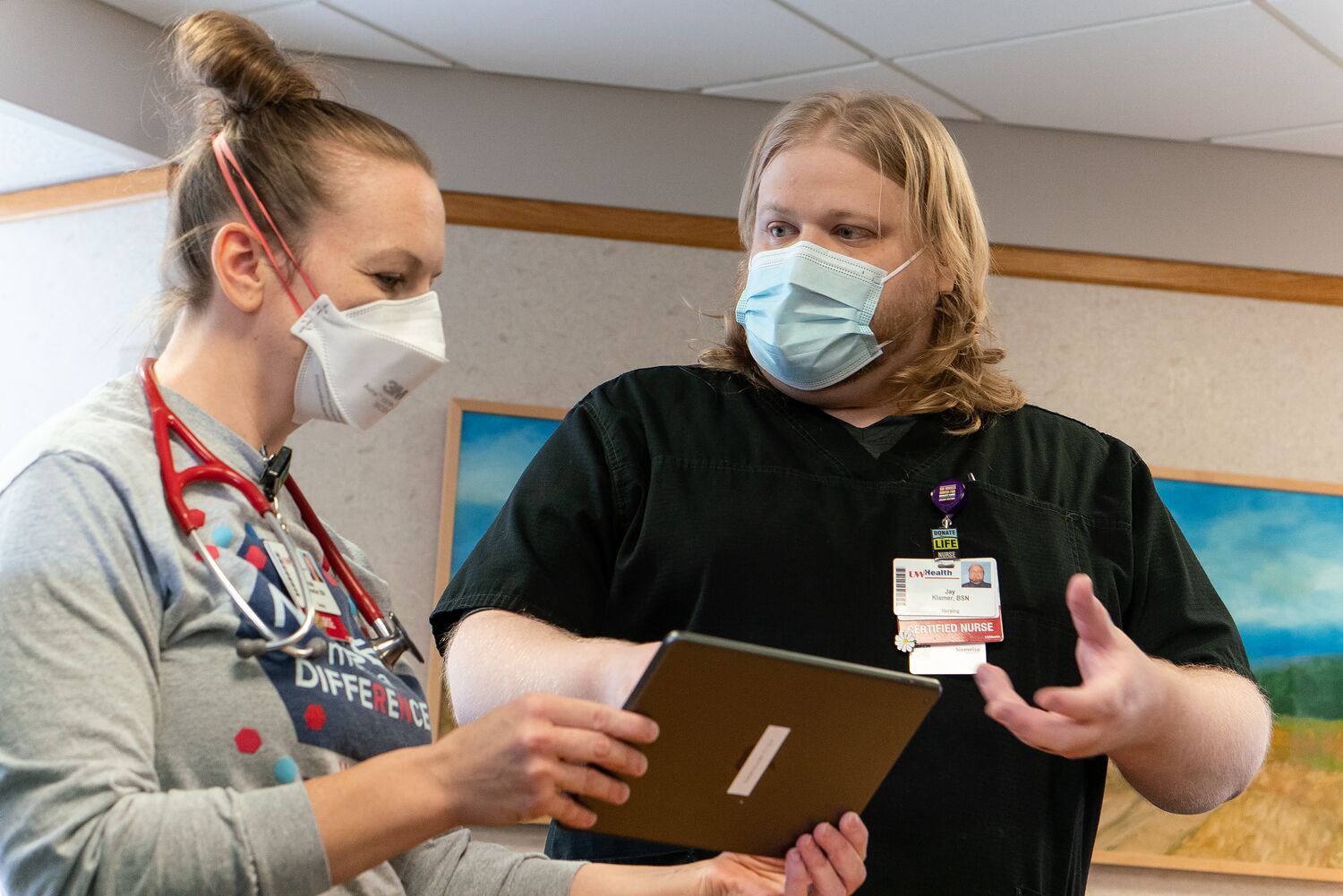
When Jay Klamer, BSN, RN, started working on the Transplant Unit at University Hospital, daily patient and family education sessions were held in the nearby family lounge.
“It was great because transplant patients and their support people would attend along with nurses and pharmacists,” Jay said. “The sessions were very useful because the patients and families could interact with the care team and ask questions.”
Unfortunately, that changed in early 2020 with the onset of COVID-19 pandemic. The transplant teams could no longer use the lounge, so they moved to nurse-to-family and nurse-to-patient models, which weren’t as effective.
“When there is one person instead of eight providing the education, it takes less time away from patient care. Providing all the education at discharge takes a lot more time and is very challenging for the person managing the discharge,” Jay said of the resulting strain on nurses. “It was equally difficult for patients who weren’t getting their post-hospital care education needs met because everyone was doing it differently.”
That’s when Jay knew there was a better way to help patients and his nursing colleagues.

The first attempt to fix the issue involved patients using iPads to attend a daily virtual class led by a clinical nurse specialist or nurse.
“Consistency was still a challenge and support people would often miss it due to COVID visitor restrictions,” Jay said. “So, I took a closer look at how much we were missing and wondered how we could fill in the gaps.”
Jay recalled that pharmacy had a similar issue and subsequently changed their class to a video format, which provided more viewing flexibility for patients. He realized this same approach would help transplant patients receive the education they needed, while greatly helping nurses from a time perspective.
Jay standardized the video content and engaged key colleagues, including clinical nurse specialists Gwen Klinkner, DNP, RN, BC-ADM, CDE; and Jess Viste, DNP, RN, ACNS-BC, CCTM.
“I could not have gotten this far without the help from Gwen and Jess,” Jay said, noting that Gwen ensured the language was at the appropriate medical literacy level and helped with scripting, while Jess provided the core educational content and reviewed everything for accuracy.
Although creating the videos has taken more time than Jay anticipated, he is excited to help patients and nurses once all videos are accessible via MyChart and uwhealth.org. “We have robust written versions of our materials, but there are limitations. Having this education available on video improves access for all patients and will help everyone in the long run.”
Pre-admission discharge planning is a win for patients

It’s safe to assume that no one wants to be hospitalized longer than necessary. Unfortunately, there are instances when patients are medically ready for discharge but unable to leave for an outlying reason, such as needing long-term care and a nursing home bed is not available. These are referred to as “avoidable days” and cause a ripple of dissatisfaction for patients ready for discharge and those in need of care. The cost also adds up.
Outcomes manager Katie Meicher, BSN, RN, identified an opportunity to address this preventable issue with improvements to case management workflows.

“It had been hypothesized that discharge planning before scheduled surgical admissions would provide several benefits,” Katie said. “It could reduce avoidable days as well as the number of patients turned away, while improving patient satisfaction, outcomes and hospital capacity issues,” Katie said.
To put things in motion, Katie conducted a test of change on a subset of vascular surgery patients who met the criteria of having a planned surgery. Prior to admission, they were called by a case manager for an initial interview to gather information pertinent to discharge planning, and to help set reasonable expectations for the length of stay and anticipated discharge needs. Case management was then able to start pre-admission discharge planning.
“The results were astonishing,” Katie remarked. “Not only did the six-month test of change reduce avoidable days by greater than 90%, we discovered an unintended benefit — there was more time to reprioritize patients who were urgently admitted but had at least 24 hours before going to the operating room.”
With the prioritization of those patients, the vascular surgery case manager was able to begin discharge planning pre-operatively, thereby reducing avoidable days in that population by greater than 90% as well. The estimated annual financial impact of this intervention was a reduction in cost of $245,813 with a projected reduction of over $3.1 million annually once scaled across surgical services.
“Follow-up survey data also revealed that the patient experience had been overwhelmingly positive regarding the reduction of avoidable days and improved patient communications,” Katie said. “With further reduction of avoidable days, we project that bed availability will increase, benefitting patients in need of quaternary care.”
Check out more stories featuring the great work of our nurses in the 2022 Nursing Annual Report (pdf).
