Caring for Patients on Their Worst Day
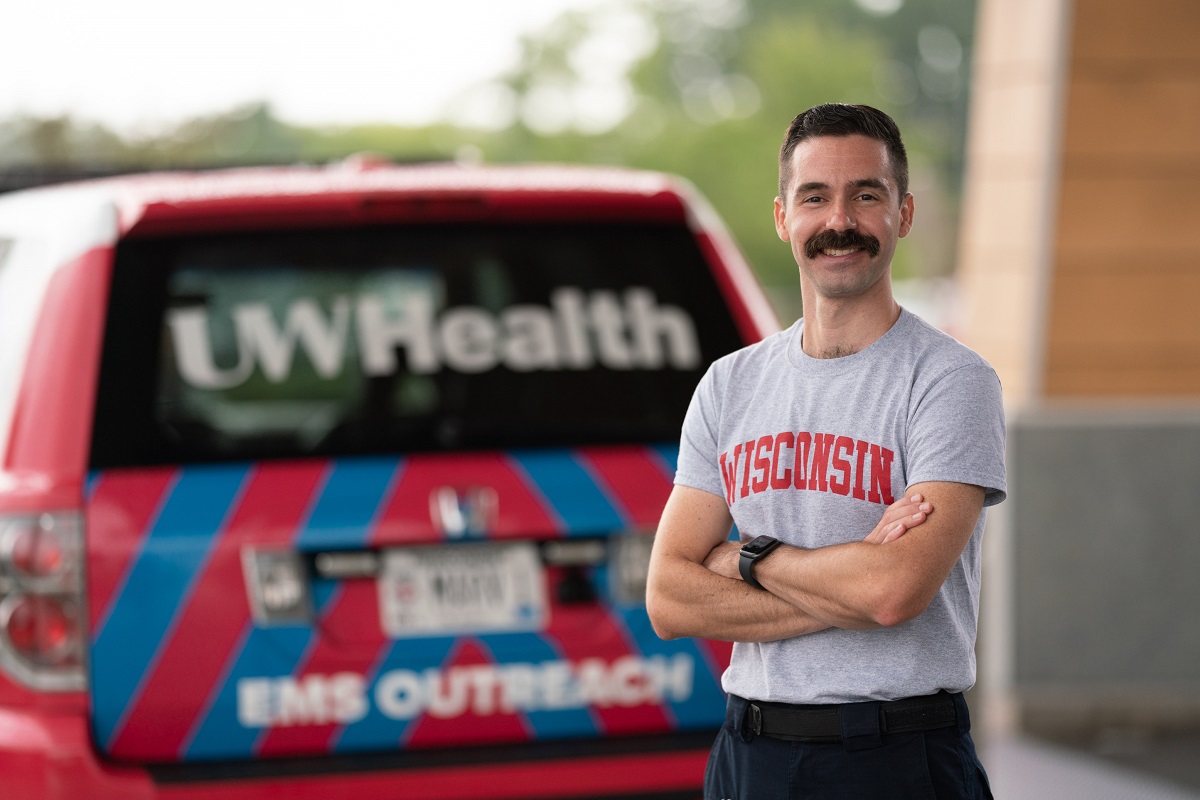
APP Champion: Mike Horowitz, PA, Emergency Medicine, University Hospital, East Madison Hospital
Mike Horowitz has always loved emergency medicine. It’s fast paced, unpredictable, requires astute assessment skills, flexibility and the ability to function in a high-stress department. Working as an EMT/firefighter in the past, Mike says emergency medicine just comes naturally to him, maybe even instinctual. “It’s always been my home base. I’m often seeing a patient on their worst day. My day-to-day is their worst day.”
Mike is a physician assistant (PA) in the emergency room, working at both University Hospital and UW Health at The American Center. He’s been with UW Health for five years. About a year ago, he took on the role as assistant medical director for Waunakee and Sun Prairie emergency medicine services (EMS). He assists with education and training for physician assistant students, prehospital providers and advanced practice providers.
Mike became a physician assistant in 2013 after earning his Master’s of Physician Assistant Studies at Drexel University and 18-month postgraduate residency program in emergency medicine at Einstein Medical Center Philadelphia.
PAs are medical professionals who diagnose illness, develop and manage treatment plans, prescribe medications and often serve as a patient’s principal healthcare provider. With thousands of hours of medical training, PAs are versatile and collaborative. They practice in every medical setting and specialty, improving healthcare access and quality.
Mike also pursues his passion for emergency medicine by volunteering as a medical provider for a local street medicine program called Madison Area Care for the Homeless OneHealth (MACH OneHealth). With compassion and respect, the organization works to bridge gaps in area healthcare systems by connecting with people experiencing homelessness. “We bring medical attention, preventive care and acute care services to local homeless populations,” Mike says. “I visit Madison homeless shelters about once a month or every other month, about 3–4 hours each time.”
Mike says MACH OneHealth helps with whatever is needed, such as chronic illness management, primary care, general health concerns or acute medical issues. “We often work with them to avoid hospitalizations, and if they do need emergency attention, we refer them to the emergency department (ED) and work together to coordinate that care. We advocate for housing and general health and wellness. It’s totally independent and volunteer funded. It’s really rewarding work.”
Teamwork is essential in the ED. In fact, when Mike was asked to describe his teammates, he says teamwork and people are really the crux of how the emergency department works. “Rarely is the emergency room the definitive care for a patient. But there are times when it is, and that is one of the reasons why I’m in medicine. We can be the safety net for those patients. I discuss cases with other providers and work to transfer patients for specialized care. Sometimes it takes several phone calls to outside agencies or other units, depending on what they need. There are a lot of great people within UW Health who really want to get involved in their care.”
Mike says his colleagues are a pleasure to work with. “Not enough can be said about how great the emergency room staff are—they are fantastic. The heart of a high-functioning healthcare organization is the team element. The emergency room is a well-oiled machine.”
The intensity of an emergency can provide a memorable moment for anyone, whether you are on the giving or receiving side. “I can’t recall a specific experience but maybe a cumulative experience,” Mike says. “Critical care, street medicine and emergency care are all that I do. One of the reasons I went into medicine was to have the fluidity of working in that environment. My mission as a physician assistant is to serve the underserved. That has kept me grounded. Caring for a patient who has no place else to go. Helping them navigate the healthcare system—sometimes it’s a real struggle—I’ve found that many times my role can be very helpful with those aspects of care.”
Mike says his patients have taught him how to stay humble because things can often surprise you in medicine. “Emergency medicine can become depersonalized with medical issues glossing over the personal aspects of a patient. My patients have taught me not to lose any thread of humanity,” he says.
Mike understands that patients have emotions and fears. Many times, he works with a patient’s family to help in the care process. “Sometimes patients lack income and/or other resources, so I like to help them find the resources they need for care. These issues all impact the way they see their care. If I don’t take a moment to learn about a patient and their frame of reference, I’m doing them a disservice.”
