
Over the past few years, the ongoing challenge of capacity constraints has impacted general care units at University Hospital, requiring adjustments in nurse-to-patient staffing ratios to accommodate the increase in patient acuities and specialty patient populations. Although the goal has always been to staff to meet the needs of all patients, the adjusted models lacked consistency across units.
Early in 2023, inpatient RNs within the medical/surgical nursing division expressed dissatisfaction with disparities in the adjusted staffing ratios, conveying an increase in workloads due to their challenging patient populations.
Pivotal feedback from RNs
To assess the situation, nursing leaders included staffing ratios as a consistent topic of conversation with direct care RNs during regular rounding — especially those working night shifts — who were experiencing the highest level of dissatisfaction due to their nurse-to-patient ratios changing from 1:4 to 1:5 based on demands.
“Some units decrease RN staffing for night shift,” said Alysia Hanson, DNP, RN, director of medical/surgical nursing. “Nurses provided important feedback that it had become more challenging to decrease staffing on night shift given the increasing acuity of the patient population at University Hospital.”
In addition to the feedback obtained during rounding, direct care nurses on general care units performed data collection for one week to determine if 1:3 RN-to-patient ratios might be needed based on a specified rationale that involved a list of 13 patient scenarios and care needs.
“Unlike intensive care units where they have criteria to determine when a 1:1 ratio is required, there isn’t a consistent mechanism to account for increases in staffing needs based on acuity on general care units,” Alysia said. “When the nurses performed the data collection, it revealed that staff felt 35.8 patients per day (across general care units), required a 1:3 ratio.”
RNs shape the change
Based on the feedback, the assessment (which included benchmarking data) and other data collected by staff, a baseline acute care matrix was developed and implemented on four medical/surgical units that had been consistently staffed with ratios of 1:4-5 on night shift. The result was an addition of 6.4 RN FTE across night shift teams on the four units. In addition, there was continued support for leveraging acuity-based staffing logic within Health Link, the electronic medical record.
The General Internal Medicine Unit was one area that experienced the staffing improvement. Courtney Harvey, BSN, RN, care team leader, comments on the positive effect it had on nurse satisfaction and night shift morale.
“Having another RN added to our night shift has been a huge benefit to all. Our nurses have had more time to spend at the bedside and are able to address the needs of our patients in a timely manner,” Courtney said. “As a care team leader, this change also allows me to spend more time supporting our newer staff and serving as a resource to all, especially during unpredictable situations or events that may occur throughout a shift. Overall, this has been an incredibly welcomed staffing reform for our nurses. I am so thankful our voices were heard and that our staff have felt such a positive impact from this exciting change.”
What comes next
The vision for this work spans into fiscal year (FY) 2026, with the goal of leveraging the Health Link workload scoring tool in 2024. Additionally, there will be ongoing efforts to reassess the level of care criteria as we look forward to the opening of the D2 tower and increased capacity.

Check out more stories featuring the great work of our nurses in the Nursing Year in Review 2023 (pdf).
Helping military veterans obtain civilian health care roles
In September 2023, Kelly Wheeler swapped her U.S. Navy corpsman uniform for medical scrubs as a medical assistant tech at UW Health. Kelly works at her hometown clinic in Cottage Grove, Wis., giving vaccinations, taking blood pressure and other tasks to assist providers.
It was a job she did not think was possible right out of her military service, despite spending the last seven years performing similar medical tasks such as dispensing vaccines, analyzing lab samples and assisting in surgeries as a Navy corpsman. That’s because in most states, military health care experience cannot be applied to civilian health care roles due to credential and licensing requirements.
But in 2022, the Wisconsin legislature approved the Wisconsin Military Medics and Corpsmen Program. It waives the credential and license requirements, allowing eligible Army medics, Navy corpsmen and Air Force techs to work in civilian health care roles under supervision while they seek medical credentials or licenses.
The legislation was championed by a nonprofit group called Heroes for Healthcare. They are leading the effort and partner with health systems such as UW Health to help medically trained veterans and military personnel transition into civilian health care roles.
“It’s a win-win for veterans and health care systems like ours,” said Rudy Jackson DNP, MHA, RN, CENP, chief nurse executive, UW Health. “We can build our workforce amid a shortage of workers while helping medically trained veterans and military personnel transition into civilian health care roles.”
Kelly became the first participant in the program. UW Health created a position for her to work three days a week while attending nursing school online two days a week.
This effort is personal for Rudy, who spent 27 years in the Army primarily as a medic and nurse for patients in a war zone, but right out of the military he worked at Blockbuster Video because his military training did not translate to a civilian health care role.
Fortunately, that has now changed and UW Health leads in this innovative space by providing opportunities for these trained, hard-working medical professionals who want to help people in their communities.
This program has been accepted by the American Organization for Nursing Leadership (AONL) and will be presented at the national AONL conference in 2024 by Anne Mork, MS, MHCDS, RN, chief nursing officer, ambulatory and nursing support services; Luke Sticht, MSN, RN, CENP, CCRN-K, chief nursing officer American Family Children’s Hospital; and Shabvon Johnson, BSN, MBA, RN director, ambulatory operations.

Check out more stories featuring the great work of our nurses in the Nursing Year in Review 2023 (pdf).
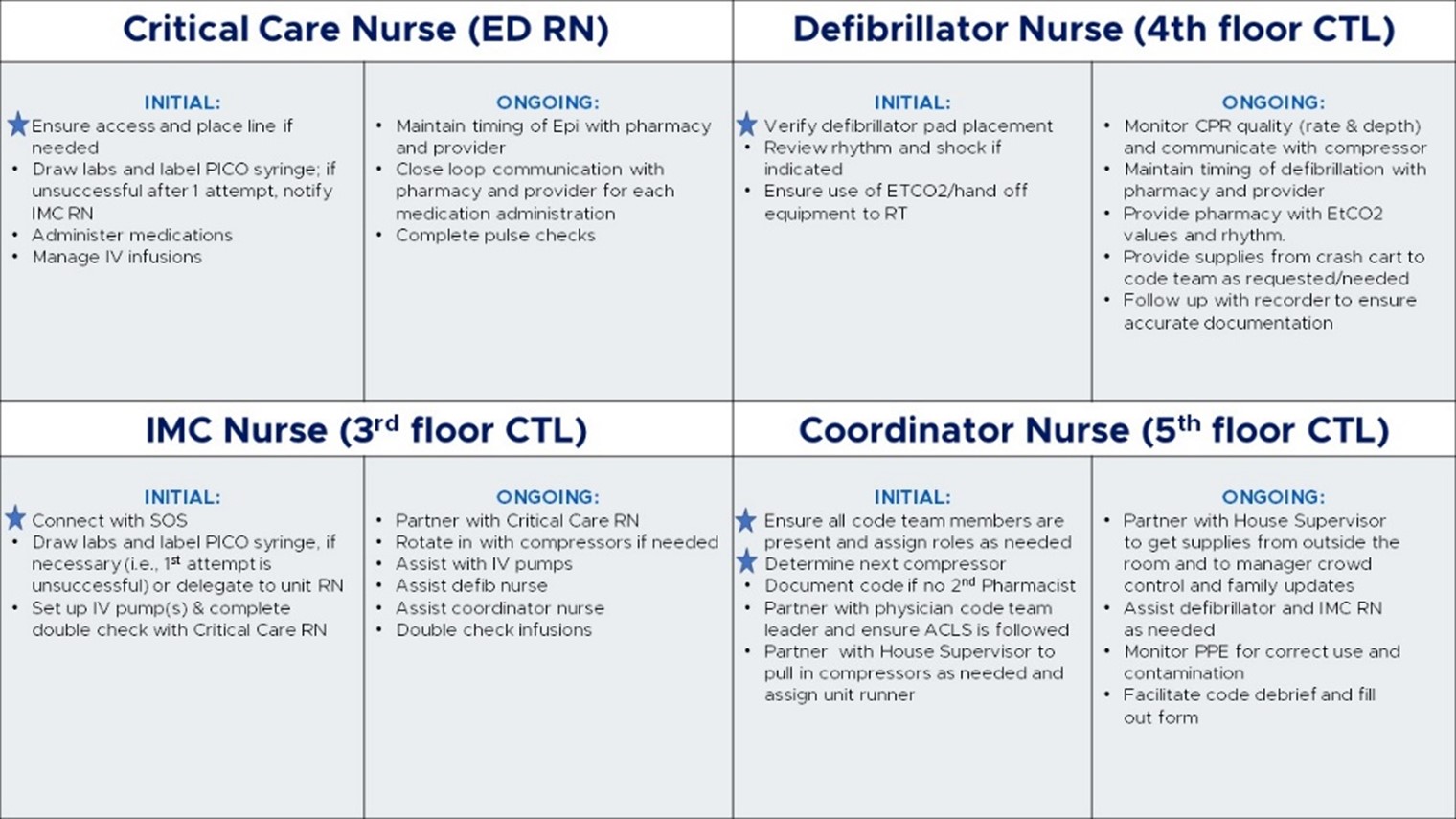
RN code roles bring confidence

In the inpatient environment, it’s inevitable that nurses will experience a code at some point. While an understandable amount of stress accompanies the team that flies into action, having a well-orchestrated process can help curb some of that anxiety.
And that is exactly what Laurel Mitmoen, MSN, RN, nursing education specialist, set out to do when she created specific RN code roles.
“When we saw University Hospital pilot the RN code roles with great success, we immediately wanted to adopt the practice at East Madison Hospital,” said Kristen Stine, nurse manager. “Because we don’t have a lot of codes on our inpatient units, the staff has expressed unease and asked for more education and direction.”
Laurel was happy to help.
“I thought it was a great idea because there are so many benefits to adopting the standardized model,” Laurel stated. “Codes can be understandably chaotic — there’s no pulse, no breathing — and advanced lifesaving care is needed. Having defined roles for each person involved, brings some calm to the process and helps RNs feel more confident, knowing what they’re expected to do when they get in the room.”
Because the shifts and volume of resources vary at East Madison Hospital — day shift to night shift and weekday to weekend — the challenge was to establish standardization and structure that would meet all shift needs with the available resources. Four established code roles and associated tasks helped achieve that:
- Critical care nurse (emergency department RN)
- Defibrillator nurse (4th floor care team leader)
- Intermediate care nurse (3rd floor care team leader)
- Coordinator nurse (5th floor care team leader)
To prepare for the new roles, Laurel, Kristen, along with Andrea Mckenna, clinical nurse specialist at East Madison Hospital, developed a training program that includes interdisciplinary mock codes. The program went live in September 2023, therefore, specific outcome data is still being collected given the low number of codes at the hospital. However, as a result of the training, nurses demonstrated a 37% increase in knowledge in locating critical supplies and a 19% increase in awareness of code leader roles.
RNs who attended the training also provided positive feedback about the value of the training, being able to go through the code cart and how the training content applied to real-life experiences.
“These defined roles have allowed our nurses serving in code roles to have more focused tasks during a stressful situation, which will likely translate into increased confidence and hopefully strong patient outcomes,” Kristen said.
Check out more stories featuring the great work of our nurses in the 2023 Nursing Year in Review (pdf).
Inventive approach to allied health visits

When the COVID-19 pandemic hit in 2020, UW Health flew into action like most health care systems, devising new ways to care for patients and employees in the safest way possible.
One of those efforts was establishing a COVID-19 testing drive-thru site to provide additional access for testing and reduce foot traffic and exposure in clinics and emergency departments. Once COVID-19 vaccinations became available, the drive-thru continued to serve that purpose, and the realization set in that this convenient option could benefit patients and staff in other ways too.
“We received a lot of positive feedback from patients and employees about the drive-thru process, especially parents who enjoyed the convenience of keeping their children in the vehicle rather than going to a clinic,” stated Linda Yim, RN clinic manager, UW Health vaccine clinics. “So, we started to explore how this model could be used long-term to help our primary care colleagues who are often overwhelmed by high patient volumes and low staffing.”
As a pilot initiative in July 2023, the John Wall Drive site started incorporating routine vaccinations (tetanus, hepatitis B, shingles, human papillomavirus infection), seasonal vaccinations (COVID-19, influenza, respiratory syncytial virus (RSV for adults), and testing (influenza, RSV and strep) to provide additional access and divert these visits from primary care clinics while also improving vaccination rates for kids.
“Leaders evaluated the impact of the pilot in early 2024, to determine what a long-term model might look like,” Linda said. “We implemented a soft rollout of additional services in early 2024 including blood pressure checks as well as contraceptive and vitamin B12 injections. If we sustain the drive-thru model, our future state may include durable medical equipment, wound care, supplies and vaccinations for children under 5 years old.”
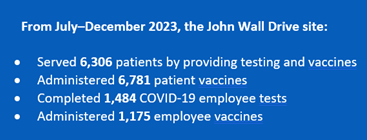
Positive impact on workforce
With the advent of the drive-thru site in 2020 came the addition of a new clinical support technician (CST) position that was created based on the associated demands.
“This role was a great way to attract people interested in health care with no clinical background because they’re trained on the job by RN leads,” Linda said, noting that although the CSTs are limited in what they can do — mostly swabbing and vaccinating under RN lead supervision — these roles have continued to be a huge asset in providing services to patients. “It’s also great to see the retention and growth among CSTs as many of them are staying with UW Health and taking advantage of the career pathways offered, such as the Medical Assistant Apprenticeship Program.”
In addition to the CST role, the position of lead site RN — initially filled by travel nurses early in the pandemic — was carried over from the testing team that Linda started overseeing in May 2023.
“We had two lead site RNs come on board in late 2023; one was a new hire and the other transferred from one of our clinics,” Linda said. “Both the RN lead and CST positions began as temporary roles that transitioned to permanent roles, which was great to see.”
The drive-thru site also employs 16 RN clinical support staff in part-time capacities (1–2 days per week), but Linda hopes to have these positions become long term in 2024 to support the site’s growing list of services.
Check out more stories featuring the great work of our nurses in the 2023 Nursing Year in Review (pdf).
Family ties to health care and UW Health

Nursing is a profession deeply rooted in compassion, care and dedication to the well-being of others. For families like Christine Abong’s, this call to serve is a shared family trait.
“You are in nursing because you want to help and make a difference,” said Christine, MSN, RN, CNN, and inpatient dialysis manager, UW Health. “I tell my children that it is a calling, because if you don’t have those traits, you won’t be in this profession very long.”
Christine, a UW Health nurse for the past 20 years, has two children following in her footsteps. Daughter Frances Christylle is in her first year as a nurse resident in perioperative services, while her sister, Katrina Ella, started as a clinic nurse resident at EMH Orthopedic Clinic in February.
Her daughters’ career choice was not something Christine ever saw coming when she became a UW Health nurse two decades ago. Growing up in the Philippines, she was drawn to a job in health care, but after putting herself through college, realized she would have more opportunities as a nurse if she moved abroad. So, in 2003, Christine moved to Madison with about 30 other aspiring nurses as part of a partnership between UW Health an agency.
Christine was assigned to work for UW Health, so she and her husband, Francis — a UW Health medical assistant — moved to Madison and settled in before bringing their three young children with them the following year.
As Christine delved into her nursing career, her dedication to patient care became evident to everyone around her — including her daughters. Witnessing their mother’s compassion and the impact she made on people’s lives, Katrina Ella and Frances Christylle chose to embark on their own nursing journeys. They both travelled to their parents’ home country to study nursing and have recently returned following graduation.
“It was really our Nurse Residency Program that brought them back here,” Christine said. “They’re able to be in a learning program where they’re protected and are getting great experience with a holistic approach to health care.”
Her daughters’ decision to become nurses has filled Christine with pride. They share a familial bond and a passion for healing, which further strengthens Christine’s commitment to making a positive impact in health care.
“I try to be honest with my children and tell them that nursing is not an easy job, and it’s not for the weak of heart,” Christine said. “Your schedule varies, you work nights, there is a lot of learning and a lot of stress because you are dealing with human beings and lives.
“But you get to take care of someone and give kindness and compassion. It’s about making connections and being appreciated. When you see what your actions can do for someone else and they are appreciating you, you’ve already won, because you are making a difference in their lives. You’re connected to a life. And I’ve tried to teach my children that.”
Check out more stories featuring the great work of our nurses in the 2023 Nursing Year in Review (pdf).
On the leading edge of technology: Generative AI in nursing

UW Health is committed to leveraging technologies to ease the demands nurses face every day. Early 2023 saw the rise of a revolutionary technology — generative artificial intelligence (AI) — and the potential it has in transforming the delivery of patient care, improving operational efficiency, reducing cognitive burden and streamlining administrative processes.
In April 2023, UW Health entered a partnership with Microsoft and Epic Systems introducing generative artificial intelligence (AI) to the organization as a unique development opportunity to explore within health care, and specifically in nursing care.
The complexities of considering the use of generative AI at UW Health have required a thoughtful and strategic approach to determine how best to apply this advanced technology. “Generative AI is evolving at a rapid pace and will be widely adopted in the years to come,” said Becky Kohler, MPH, RN-BC, chief nursing information officer. “Within the profession of nursing, this technology requires a proactive RN influence and active RN voice to ensure it is a safe, effective and meaningful solution.”
UW Health as an early adopter
In the past three years, the rise in virtual health care visits has caused an increase in the use of digital communications in health care. According to a study in the Journal of the American Medical Informatics Association, the volume of electronic messages sent to health care providers has increased by 157% compared to pre-COVID levels. In 2022, UW Health administered a survey to obtain end-user feedback on Health Link (electronic health record software powered by Epic). The message volume in the In Basket communication hub (used to send and receive messages) was one of the top items clinicians asked to be addressed.
In September 2023, the first cohort of UW Health ambulatory nurses started a trial use of generative AI in the ambulatory clinic setting within the In Basket section of Health Link. The specific AI technology used in this instance is a large language model (LLM), which enables users to refine and steer a conversation toward a desired length, format, style, level of detail and language. For this trial, when a patient sends a message to the care team, the LLM (via ChatGPT software) generates a recommended nursing response instead of the clinic RNs manually typing the responses. Clinic nurses tested this model and provided valuable feedback on the functionality.
“Nurses are guiding and leading the use of this very new and emerging technology,” said Shelly Key, RN manager, Health Link and ambulatory operations. She explained that the testing process involves nurses using the LLM responses in their day-to-day work by watching for incoming messages from patients via MyChart, and determining if the generated AI response is helpful. “Some of the data we’re collecting is showing that nurses are using the technology more than providers, and are using at least half of the generated message.”
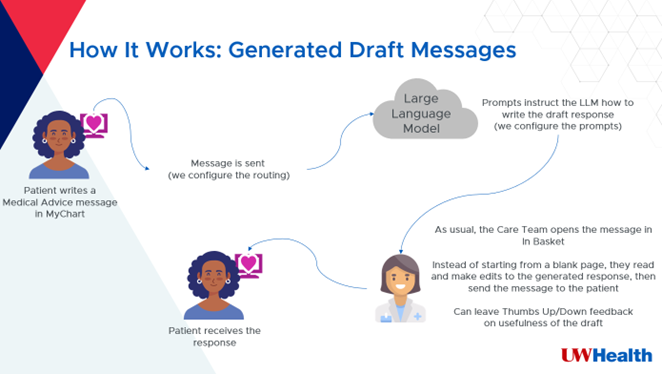
Nurses help shape the technology
While the technology is showing promise in creating a more efficient process, the role of the RN is vitally important. Nurses apply their clinical expertise and judgment in reviewing each message to determine if it’s accurate, needs editing or should be discarded and completely rewritten.
“Nurses who are trialing the technology send real-time feedback to the team along with the themes they’re seeing,” Shelly said. “We collect that information, share it with Epic and work with them to enhance the tool. All of this is being done in a controlled manner — monitoring it closely and regularly engaging clinical team members for feedback — to make sure it’s safe and effective.”
The goal for 2023 was to partner with nurses in the development and creation of a safe and effective tool that can be seamlessly integrated into the nursing workflow.
Future opportunities for nursing
It is important that nurses continue to be part of the development and trial of generative AI solutions so that the unique workflows and considerations of nursing practice and licensure are factored in.
“Partnering in the In Basket trial opens up doors for what’s coming in 2024,” Becky said. “In early 2024, a handful of inpatient nurses will trial generative AI to draft end-of-shift notes. We wouldn’t be able to advance this leading-edge work and technology without nurse involvement, which speaks volumes to the incredible value of RN voices.”
Check out more stories featuring the great work of our nurses in the 2023 Nursing Year in Review (pdf).
2024 UW Health Nurse Excellence Awards
Congratulations to our 2024 honorees and nominees. Hear from each award recipient as well as family members and colleagues of Nichole Warner, who honor her memory and the lasting impact she made.
Meet our 2024 Nursing Excellence Award recipients
 Korben Bergmann Health Unit Coordinator Trauma & Life Support Award: Support Staff-Nonclinical |
 Marcia Foltz, BSN, RNz Inpatient Imaging University Hospital Award: Surgical & Procedural Services |
 Kayla Foster, BSN, RN Inpatient Operating Room American Family Children’s Hospital Award: Rising Star |
 Corey Gilbertson, BSN, RN Cardiovascular Cardiothoracic Intensive Care Unit University Hospital Award: Intensive Care Units |
 Kayla Kenney, BSN, RN Heart and Vascular Progressive Care Unit University Hospital Award: General & Intermediate Care |
 Megg Kohel, BSN, RN Integrated Care Programs Yahara Clinic Award: Primary Care |
 Kelli Linderman, BSN, RN Transitional Care University Hospital Award: Patient & Care Coordination |
 Morgen Makela, CNA Medical/Surgical Unit, 3rd Floor East Madison Hospital Award: Support Staff-Clinical |
 Courtney Schultz, BSN, RN Pediatric Specialty Clinics American Family Children’s Hospital Award: Pediatrics |
 Gina Tranel, MSN, RN Clinical Simulation Program University Hospital Award: Leadership and Advanced Practice |
 Jennifer Vivian, BSN, RN Pediatric Universal Care Unit American Family Children’s Hospital Award: Preceptor/Mentor |
 Nichole Warner, BSN, RN Infectious Disease Clinic University Hospital Award: Specialty Care In memoriam |
 Susanne Wolfe, BSN, RN Emergency Medicine University Hospital Award: Emergency Services |
Nurse Excellence Award nominees
UW Health recognizes all nominees for their valued contributions to professional nursing practice and patient care.
| Diane Aide Lyvia Aide Zach Anderson Mary Jo Arcand Kayli Austin Melissa Beltran Jada Berg Korben Bergmann Annie Berousek Allie Biba Kimberley Boehm Jessica Branson Andrea Briese Elizabeth Cabus Kay Caldwell Holly Casson Stephanie Chatelain-Taapken Jon Chmielewski Kaitlin Collins Brianna Colvin Kamilee Conaway Chelsea Cornelius Chad Courtney Maria Duran Contreras Jack Eder Salvador Enriquez Andrea Esparza-Monroy Kathy Farwell Katrina Fingerson Erin Fischer Samantha Fitzpatrick Catherine Fleiner Marcia Foltz Katie Forseth Kayla Foster Breanne Fourtner Elizabeth Frederick Meghan Furstenberg-Knauff Sherry Gahagan Kevin Geen Corey Gilbertson Amancio Gonzales Robyn Gunderson Kaci Hanewold Hillary Hanna Crystal Hartmann Courtney Harvey Steve Hill Jenny Hobson Meghan Holum Christina Hull Kayla Hunt Anne Iverson Kiana Jaramillo Brittni Jegerlehner Jen Kakuske Kayla Keeney Katie Knaggs Kirsten Koffarnus Megg Kohel Laura Konkol Lara Leroy Denise LeRoy Yangchen Lhamo Kelli Linderman | Hayley Lindsey Jennifer Liter Anna Loken Emily Lynch Alexander MacDonald Kim Maerz Morgen Makela Jill Markus Wendy McKnight Taylor Mikulsky Jennifer Moore Margaret Murray Andrew Navarro Julianne Norcia Jenny Pauley Marcia Pauls Ashli Paulson Sarah Peck Nastassja Petermann Stephanie Peterson Stephanie Prahl Kristi Probelsky Klaire Provos Zac Rakke Lauren Reible Kathy Rozema Judith Rufener Luther Rundell Ali Sabers Sarah Schaan Hailey Schiro Chrystina Schroeder Courtney Schultz Sonya Schwanke Alyssa Seamonson Joleen Semmann Lisa Semmann Gladys Serrano Martinez Eva Sharp Reade Shenk Janet Shimniok Jenna Shinstine Courtney Skaife Josefina Slack Amy Smith Brittani Stankevich Andrea Stapelman Kristin Strampe Jessica Swanson Jenna Torgeson Gina Tranel Emma Rose Traxler Julie Trowbridge Kelsey Turner Valerie Van Horn Jennifer Vivian Nichole Warner – in memoriam Amanda Weber Kathy Wilstein Cammi Wolfe Susanne Wolfe Mao Xiong Frank Yokosh Ryan Ziegler Kayla Zubke |
UW Health RNs shine on international stage

In celebration of UW Health Wisconsin receiving its fourth Magnet designation in 2023, a group of UW Health RNs and leaders from Wisconsin and Illinois attended the 2023 international Magnet Conference where this incredible achievement was recognized among 13,000 nursing peers from 27 countries.
At the conference, UW Health nurses shared an impressive quality improvement project and gave two impactful presentations—one of them receiving a standing ovation—further demonstrating that UW Health nurses are true experts and international leaders.
Nailed it! Shared governance presentations wow audiences
As part of the educational sessions offered throughout the Magnet conference, UW Health shared two presentations that highlighted impressive elements of how UW Health got to where it is with its effective and evolving shared governance structure.
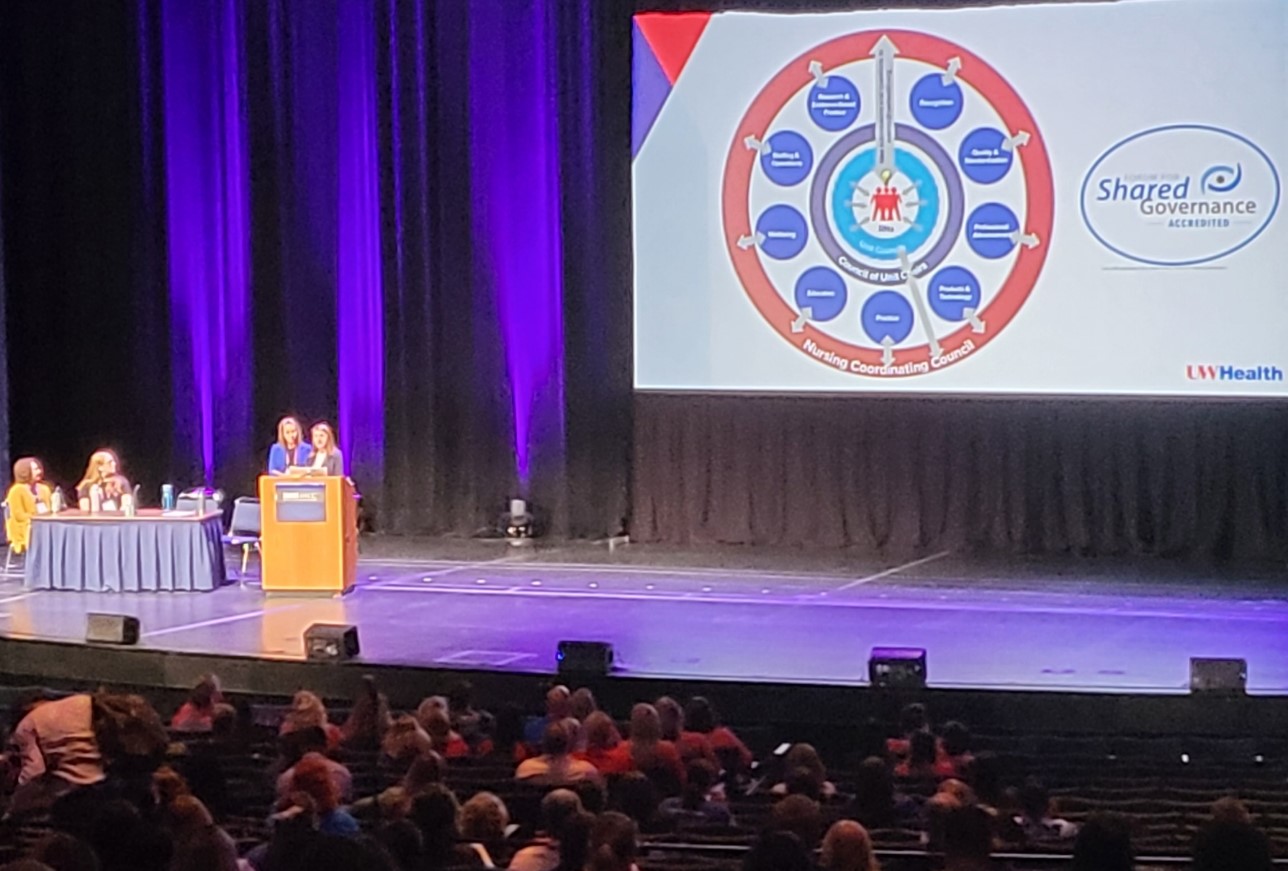
“Using Data to Optimize Shared Governance Structure and Culture” was presented by Sarah Brzozowski, PhD, MBA, BA, RN, NEA-BC, Director, Magnet & Nursing Excellence, and Pamela Blabaum, COTA, Nursing Program Coordinator-System Strategy. Sarah and Pam shared how essential is it to leverage shared governance in today’s work environment, by bringing direct care nurses and leaders together to make decisions and drive outcomes. In addition, they showed how UW Health has optimized its shared governance council structure to enhance the confidence and influence of nurses throughout our organization.
“Structural Empowerment through Nursing Unit Councils”was presented by Mark Ravis, BA, RN, PMH-BC, MDiv, Care Team Leader, Inpatient Psychiatry, and Sarah Brzozowski, who touched on the nursing shared governance structure at UW Health, the need to optimize unit councils, how to tackle improvements and opportunities from multiples angles, as well as outcomes and next steps.
Both presentations were extremely well-received with nurses from across the nation and world, asking multiple questions after each session. One nurse who attended the Structural Empowerment through Nursing Unit Councils presentation felt compelled to share some positive feedback, stating:
“You guys rocked this presentation. This is the best session I’ve attended. Your work is really impressive.”
In addition, the founder of the shared governance accrediting body The Forum for Shared Governance, Dr. Robert Hess, was in attendance at the conference promoting the book he co-authored with Dr. Diana Swihart titled “Shared Professional Governance: A Practical Approach to Transforming Interprofessional Healthcare,” which includes a contribution from UW Health authored by Sarah Brzozowski and Mark Ravis, who shared important work that was done at UW Health on assessing the health of our councils (chapter 7). This is just another example that shows UW Health is doing amazing work in the shared governance arena!
Demonstrating quality improvement through mentorship
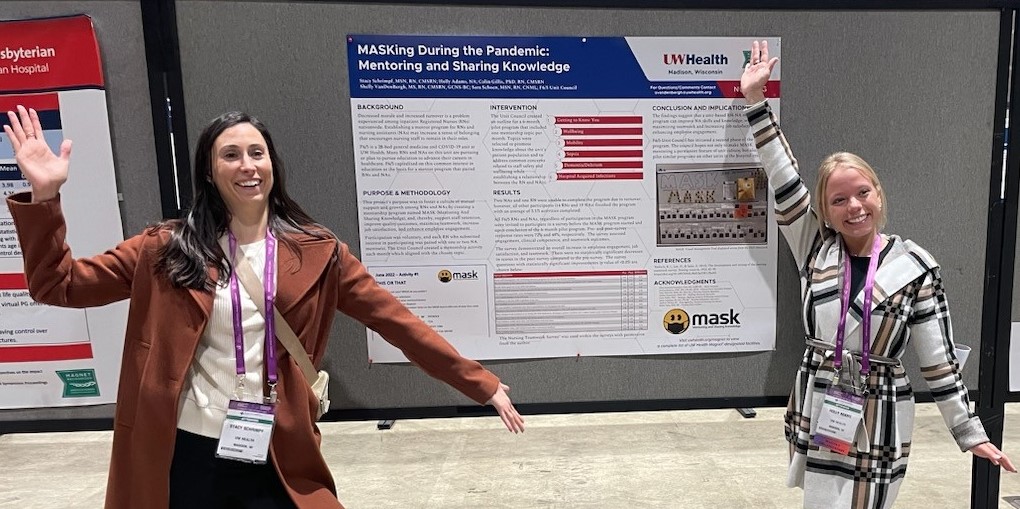
Nursing colleagues from the General Internal Medicine Unit (F6/5) at University Hospital shared their quality improvement project—“MASKing During the Pandemic: Mentoring and Sharing Knowledge”—that was designed to foster a culture of mutual support and growth among registered nurses (RNs) and nursing assistants (NAs) through the creation of a mentorship program called MASK (Mentoring and Sharing Knowledge). Through this innovative work, the unit paired RNs and NAs during the six-month program that resulted in improved NA skills and knowledge, maximized teamwork, increased job satisfaction and enhanced employee engagement.
Demonstrating quality improvement through mentorship
Nursing colleagues from the General Internal Medicine Unit (F6/5) at University Hospital shared their quality improvement project—“MASKing During the Pandemic: Mentoring and Sharing Knowledge”—that was designed to foster a culture of mutual support and growth among registered nurses (RNs) and nursing assistants (NAs) through the creation of a mentorship program called MASK (Mentoring and Sharing Knowledge). Through this innovative work, the unit paired RNs and NAs during the six-month program that resulted in improved NA skills and knowledge, maximized teamwork, increased job satisfaction and enhanced employee engagement.
Conducting Non-clinical Graduate Nursing Rotations at UW Health with a Preceptor (Practicum, Residency, Mentor)
- This resource is for students interested in doing a non-clinical rotation (also known as Practicums or Residencies or Mentorships) with a preceptor as a part of an MSN or DNP program with a leadership focus.
- Go here to determine the process for additional tracks for nursing student projects or rotations.
- All nursing graduate students (regardless of UW Health employment status) who would like to complete a non-clinical rotation with a UW Health preceptor (also known as mentor) for academic credit must follow the steps listed below.
- The steps outlined here are requirements for UW Health. There may be additional requirements from the student’s academic institution. It is the student’s responsibility to find out about additional requirements from their academic institution.
All the steps must be completed before the nursing student can begin spending hours with their preceptor as part of their rotation or participating in UW Health activities as a student. These steps ensure the student is onboarded and has completed required competencies.
Step 1. Nursing student notifies their academic institution’s Clinical Placement Coordinator
- The nursing student needs to start this process by notifying their academic institution’s Clinical Placement Coordinator to let them know of their desire to complete the student rotation at UW Health.
- The academic institution’s Clinical Placement Coordinator will ensure that an Affiliation Agreement is in place between the student’s academic institution and UW Health. If an Affiliation Agreement is not in place, it is the responsibility of the academic institution’s Clinical Placement Coordinator to complete this process. For additional guidance with this process, the school’s Clinical Placement Coordinator should reach out to NursingStudentsProjectsRotations@uwhealth.org.
- Affiliation Agreements may take 3 to 6 months to be completed. It is strongly recommended that the student inquire about this detail early in the process.
- Signing a new Affiliation Agreement is at the discretion of UW Health.
Step 2. Student identifies UW Health preceptor
- Once the nursing student receives verification that there is an Affiliation Agreement between the academic institution and UW Health, they should then find a preceptor.
- The nursing student must establish a preceptor for their rotation by identifying a UW Health employee. The student should discuss their preceptor identification with the academic institution’s Clinical Placement Coordinator and the course instructor to determine appropriateness.
- The student should work with their preceptor and discuss the student’s academic requirements for the rotation to ensure the preceptor and organization can meet their needs. The student and preceptor should create a plan to complete rotation.
- The student should review the preceptor requirements and restrictions below to be sure that they select someone who meets their rotation needs.
- If the student cannot determine a preceptor, the student should email NursingStudentAcademicProjects@uwhealth.org for help with finding a preceptor.
Carefully read and follow the requirements and restrictions of a preceptor.
Requirements of a Preceptor
A preceptor of a DNP student at UW Health will be overseeing the DNP student’s practice while they are in the walls of UW Health. Although requirements of all academic institutions may vary, a preceptor at UW Health must meet the following minimum requirements:
- A bachelor’s degree in nursing*
- Must be in a UW Health position that requires an RN as a minimum qualification. *
Preceptor Restrictions for UW Health Employees
- The UW Health preceptor cannot be the employee’s paid supervisor or manager.
- The student’s rotation cannot take place at the same location where the student is a paid employee.
- The student cannot complete their rotation hours during work hours; the student work must be completed on unpaid time.
*If the student is conducting a rotation outside of nursing, a non-nurse preceptor may be permitted. The preceptor should confirm their appropriateness with the UWH Clinical Placement Office by emailing NursingStudentProjectsRotations@uwhealth.org
Step 3. Student works with their Academic Institution’s Clinical Placement Coordinator
- Once Steps 1 and 2 are complete, the student should inform their academic institution’s Clinical Placement Coordinator so that they can place a rotation request in myClinicalExchange (MCE).
Step 4. Upload documents on myClinicalExchange
- Once the student’s rotation has been entered by their academic institution’s Clinical Placement Coordinator and approved by the UWH Clinical Placement Office, they will receive an email prompting them to upload documents into myClinicalExchange.
- The student must complete the required documentation upload and training to be compliant with the student requirements.
- Remember that this step must be completed for all nursing students, regardless of what academic institution the student attends and whether they are employed by UW Health.
- Students will know that they are compliant in myClinicalExchange when they see the green thumbs up in the system.
- Steps 1 thru 4 must be completed at least 4 weeks before the planned start of the student’s rotation
Step 5. Obtain appropriate UW Health access
- Students will receive emails from their academic institution’s Clinical Placement Coordinator and myClinicalExchange about obtaining appropriate UW Health access and a UW Health student ID badge. Once the student receives this email notification, this is the final step of this process and indicates that the student on-boarding process is complete. In coordination with their UW preceptor, the student may begin their rotation.
- Students should wear their student ID badge and always use their student login when performing student specific work.
How soon should students start this process?
- It is recommended to start the process at least 8 to 12 weeks before students are to begin their project.
- Steps 1 thru 5 must be completed 4 weeks before the first day of the student’s rotation. For example, if the rotation is to start at the end of January, Steps 1 thru 5 must be completed by the end of December. Therefore, the student should start the process in October or November.
- Step 5 must be completed before the nursing student can begin spending hours with their preceptor as part of their rotation or participating in UW Health activities as a student.
If students have questions, who should they reach out to?
Questions should be directed to their academic institution’s Clinical Placement Coordinator who will reach out to UW Health key stakeholders as needed. Students should remain in close communication with their academic institution’s Clinical Placement Coordinator.
Remarkable teamwork, remarkable outcomes
Nurses are known for their clinical expertise, compassion and humility as well as a deep appreciation for their care team members. That’s why UW Health RNs often refer to nursing as a “team sport”— to recognize the hard work of their peers and the resulting positive patient outcomes.
Ross’ surprise reunion with his nurses
Following a harrowing car crash in 2020, Ross Kopfer spent more than 60 days at University Hospital fighting for his life. In 2022, Ross was interviewed about his experience and expressed appreciation for his nurses. Little did he know that all his nurses were around the corner to surprise him after his interview, which made for an emotional reunion.

Kingston’s inspiring journey
When Tommy Wragg received the news in 2018 that his son, Kingston, had a rare condition at 3 months old, he never imagined the unbelievable journey that lay ahead at American Family Children’s Hospital.
When a kidney transplant was inevitable, Tommy helped manage an extensive medial protocol for several months to support Kingston while his body had time to grow. Complications arose a year later, requiring hospitalization for two years until Kingston was finally ready to receive his transplant in June 2022.

Tommy, who has been a single dad since Kingston was 10 months old, was touched by the endless compassion they received along the way from nearly 40 nurses and care team members from the Pediatric Nephrology Program, Pediatric Transplant Program, Pediatric Intensive Care Unit, Child Life services and others.
“Kingston’s relationship with his nurses is where everything came full circle,” he said. “He was no longer lacking a mom. They became family.”

Teamwork results in new life for a young mother
At 37 weeks pregnant, Darlene was infected with COVID-19. She declined rapidly, doctors delivered her baby and she was admitted to the ICU at UW Health SwedishAmerican Hospital in Rockford, Ill., where she spent two months.
Darlene continued to decline and her care team worried that she wouldn’t survive. But she continued to fight and it was determined she needed a lung transplant. Only one program would accept her: The UW Health Lung Transplant Program.
Over the next four months, a comprehensive team of caregivers worked to get Darlene strong enough to be eligible for transplant, which finally happened in March 2022. Darlene returned home 10 months after she was first hospitalized.
“It was so rewarding to see how someone as sick as she was, make it through,” said Brittany Schappe, BSN, CCRN, Cardiothoracic Surgery Unit at University Hospital. “She could finally go home, and she came out stronger.”

Performing a lifesaving procedure for the first time
In September 2022, the perioperative team at American Family Children’s Hospital received a referral for a fetal EXIT (ex-utero intrapartum treatment) procedure on a pregnant mom — something they had never done before, given that they rarely deliver babies.
“We had only heard about the procedure because Dr. Lobeck was heading a study to get a fetal program started,” said Aimee Muchie, BSN, RN, manager, perioperative services. “The procedure is needed when a baby is having developmental issues with its airway due to a blockage. If the baby is born with no intervention, it is not able to breathe.”
The operating team would need to perform a Cesarean section and meticulously control the bleeding to allow the surgeon to go into the uterus, take out the baby’s head, neck and one extremity, with the anesthesia team placing lines. The otolaryngology surgeon would then establish an airway while the baby was still attached to the mom.
“We hadn’t received any education, so we had about seven weeks to plan, order the correct instrumentation and determine what to expect,” Aimee said. Pressure mounted when they received word that the baby was having trouble and the procedure would take place two weeks earlier than expected. “We had to make it happen. If we weren’t ready, the baby would be delivered normally and likely die.”
Aimee said their team got “in the zone,” and performed the procedure successfully. The baby was then transferred to the neonatal intensive care unit (NICU). Both Aimee and Inna Lobeck, MD, pediatric general surgeon, attribute the success to the exceptional coordination orchestrated by the nurses and all teams — anesthesia, instrumentation, NICU, otolaryngology, perioperative — and all support services involved.
“It’s astonishing to think what we accomplished,” Aimee said, sharing that the team faced another fetal EXIT procedure just four weeks later and that it “went off without a hitch.”

Check out more stories featuring the great work of our nurses in the 2022 Nursing Annual Report (pdf).
