When health systems are overwhelmed with patients, as they have been across the nation for the past few years, academic medical centers such as UW Health feel the pinch even more than most. Patients continue to need care, so the challenge is moving them through the system as efficiently as possible without compromising quality of care or patient safety.
“As a regional referral center, we see the sickest of the sick,” said Jacinda Krueger, RN, a supervisor in the UW Health BerbeeWalsh Emergency Department at University Hospital. “So, in addition to the patients who walk in the door, community hospitals that are not able to care for highly acute patients send them to us. In addition, Dane County’s population is growing at a higher rate than any other county in Wisconsin.”
In just three years, combined emergency department (ED) patient volume (University Hospital and East Madison Hospital) has increased from an average of 234 people per day (October 2019) to 278 per day (October 2022) — a 19% increase. Incidentally, more pediatric patients (1,904) were treated in the ED in November 2022, more than any month in UW Health history, a likely consequence of the spike in respiratory syncytial virus (RSV) and flu cases.
Emergency department overcrowding is a hospital-wide challenge


Patient crowding in the ED is usually a sign that the entire health system is stressed.
When there are no beds available throughout the hospital, patients who need to be admitted must either be moved to temporary holding areas in the hospital, moved to hallways on inpatient units or remain in the ED taking up treatment spaces.
These patients, referred to as “inpatient boarders,” are cared for while they wait, but the situation is far from optimal. In recent years, ED staff at both UW Health hospitals in Madison have worked to creatively address the space problem while also continuing to ensure that the sickest and most vulnerable patients are given highest priority in the queue.
Lower-acuity patients, such as those who have pneumonia or influenza, are often seen in a special part of the ED, treated and discharged or admitted directly from the front end of the ED. These areas — known as CareSTART and the Flexible Care Area at University Hospital, and the Expedited Care Area at East Madison Hospital — are overseen by a physician and advanced practice provider team.
Despite having only 58 ED rooms at University Hospital, staff have increased bed capacity to more than 80 patients through use of flexible treatment areas and converted hallways.
“With the record volumes we’ve been seeing, we’ve expanded our ability to care for patients by adding additional treatment spaces and evaluating which patients can be treated in chairs,” said Didi Buckley, BSN, RN, CEN, another ED supervisor at University Hospital. “This helps us reserve beds for the patients who truly need them,” she said.
East Madison Hospital Emergency Department ‘borrows’ adjacent space


Similarly, East Madison Hospital saw demand at its ED grow by 19% between Fall 2021 and Fall 2022, continuing a trend of double-digit, year-over-year volume growth. Staff at East Madison Hospital are also creatively addressing overcrowding by making efficient use of adjacent spaces.
“Within our Universal Care Center, we’ve been able to ‘borrow’ space from the pre- and post-surgical area adjacent to the ED,” said Melanie Hankes, BSN, RN, nurse manager of the East Madison Hospital ED.
Hankes credits Lindsey Lehner, MSN, RN, CNOR, director of perioperative services at East Madison Hospital, and Samantha Madsen, MSN, RN, manager of pre/post/PACU at East Madison Hospital, for being an accommodating neighbor by making certain pre- and post-surgical beds available to ED patients when Lehner’s unit volumes decline later in the day. Similar to the steps taken at University Hospital, East Madison Hospital also prioritizes its 16 emergency beds for the sickest patients.
“Certain patients are evaluated in our Expedited Care Area to reserve our beds for those who truly need one, while sending home others who can be safely treated without being taken to a bed,” Hankes said.
While ED crowding is unlikely to significantly diminish anytime soon, UW Health staff are encouraged by early signs, despite knowing that much work still needs to be done.
“Most people are pretty reasonable and understanding,” said Jackie Payne, BSN, RN, care team leader in the ED at East Madison Hospital. “Despite the growing volumes, our door-to-doctor wait times have remained stable. Of course, we would love to see wait times go down but the steps we have taken prevented them from increasing.”
Guest services staff add calm
Knowing how stressful an ED trip can be even during less crowded times, ED staff have gone out of their way to manage expectations by informing patients about the new procedures to handle higher volumes more efficiently.
“Communication with patients as they enter the waiting area goes a long way toward keeping stress levels in check,” Buckley said. “We are also grateful to Guest Services for extending its Guest Ambassador Program to the ED at University Hospital.”
A longtime hospitality hallmark of the Surgical Waiting Area at University Hospital, guest ambassadors — conspicuous by their bright red shirts — warmly greet patients and family members, help familiarize them with the surroundings and provide a much-appreciated sense of comfort and reassurance.
“We’ll provide a blanket if someone is cold,” said Stephanie Bracken, Guest Services supervisor. “We’ll escort loved ones to the visitor waiting area down the hall, take people to the cafeteria or accompany them to their car when it’s time to leave. The goal is to enhance the guest experience in a stressful situation for both patients and loved ones.”
Check out more stories featuring the great work of our nurses in the 2022 Nursing Annual Report (pdf).
Innovative response to capacity crisis

When a significant uptick in emergency department (ED) and inpatient volumes occurred at University Hospital in fall 2022, considerable strain was placed on care teams and system capacity.
To ensure that patients were getting the care they needed in a timely fashion, UW Health nursing and coordinated care teams flew into action by reimagining how they could continue caring for the community.
As a result, they quickly stood up an Internal Discharge Lounge that opened Oct. 13, 2022, as a small test of change to move patients who were ready for discharge to a safe place while freeing up inpatient beds for ED patients and transfers.
“Inpatient care teams were initially provided information about the lounge process,” said Connie Allen, MSN, RN, director nursing operations support, who helped coordinate the effort with frontline nurses, clinical nurse specialists, nursing education specialists and coordinated care colleagues. In addition, guidance was given to staff and providers on applying a new lens to consider each patient as a possible candidate for the lounge.
“The coordination of efforts throughout our ED and inpatient units to raise awareness was outstanding,” Connie said.
Becky Lovett, BSN, RN, care team leader and diabetes resource nurse for the General Internal Medicine Unit, was the first staff member to send a patient to the internal lounge.
“I had been in communication with the patient’s nurse, and together, we determined that the patient was eligible for transfer to the lounge,” Becky said. “The patient’s ride wasn’t coming until 4 p.m. that day and we got her to the lounge by 11 a.m. Connie was there and two of our nurse managers, Troy Betts and Amanda Toberman, escorted the patient to the lounge, which was so wonderful and kind.”
Becky admitted to hiccups along the way, but remembered wise words from the University Hospital CNO, Michele McClure, who said: “Don’t let perfection get in the way of progress.” And they didn’t.
“The communication and collaboration were seamless, as everyone pivoted left and right to make it happen,” Becky said. “Everyone worked together to figure it out as we went along. Being nimble is so important. We got a lot accomplished — the lounge was a fantastic idea.”
This innovative approach complements the existing External Discharge Lounge, located at the Best Western InnTowner hotel, which has been serving as a transitional option for University Hospital patients and families.
“We were extremely pleased to see the success of this effort in helping free up inpatient beds to ensure patients were receiving the right level of care at the right time,” Connie said. “Although our capacity issues continue to be concerning, this key improvement helps curb the strain.”

Check out more stories featuring the great work of our nurses in the 2022 Nursing Annual Report (pdf).
We couldn’t do what we do without them

While their responsibilities are different, the staff who support nurses and patient care have some things in common: they appreciate the trust the nurses have in them, are compassionate in caring for patients, and they find even the smallest task rewarding. Another common thread they share is that nurses rely on them and appreciate the invaluable support they provide, which allows them to focus their energy where it’s needed most.
Dawn Cleary, medical assistant

When Dawn Cleary walks through the door to perform her duties as a medical assistant (MA) she feels respected by her colleagues.
“The nurses and other providers are always willing to help, they’re easy to approach and I am always learning from them,” Dawn said.
Dawn became an MA in 2015 after working for years in a completely different field at another area employer. She went back to school, drawn to help others through health care.
“There is always something to do, and I get to interact with patients and make connections with them and the other staff,” Dawn said.
Among her tasks as an MA at the Odana Rd Clinic, Dawn prepares exam rooms and patients for examination, takes vital signs, documents allergies and medications, assists with minor procedures, performs EKGs and bladder scans, administers vaccines and other injections, keeps track of forms, responds to MyChart messages and processes prescription refill requests.

Dawn also helps train students and new employees or use her expertise on a larger project.
The daily structure provides stability, but every day is different. “The most difficult part of the job is responding to unexpected clinical and administrative emergencies while maintaining professionalism and patience,” Dawn said. Most importantly, Dawn looks forward to going to work. “While some days are rough, I remember I can’t control everything, and I have a great team of people around me who support each other.”
Don Mai, nursing care partner

No two days are the same for Don Mai. As a nursing care partner his work has varied from delivering meal trays to holding a 6-month-old baby, from playing card games with a 20-year-old patient to sitting with a middle-aged patient in the emergency department (ED).
“I enjoy my job because I get to help our staff with the smallest things that can make their days easier, such as turning over rooms in the ED, running things to different locations in the hospital, answering phone calls and call lights and restocking supplies on the unit,” he said.
For most of the shifts, Don experiences something new often with a new care team in different departments. “This is extremely exciting and motivating for me as I get to learn new things about the medical field,” Don said.
Don is channeling that experience and applying to medical school in 2023 to advance his career.
Naomi Massey Haas, health unit coordinator

After many years working as a health unit coordinator (HUC), Naomi Massey Haas continues to learn something new almost every day. “I frequently run out of time to delve further into my never-ending wish list of opportunities to improve our workflow and processes,” Naomi said.
Naomi works at American Family Children’s Hospital on P5, the Pediatric General Medicine/Surgical Unit.
“A health unit coordinator serves as a bridge between a unit’s nursing staff and colleagues across UW Health,” Naomi said.
Through communication and quick problem-solving skills, HUCs anticipate the needs of team members providing direct patient care. “We have a go-with-the-flow attitude and need to be quick on our feet to support the team as patient conditions change rapidly,” she said.
Naomi credits leaders who encourage the HUC team to share ideas about improving workflow and increasing efficiency. “We get to apply our diverse skills, create new work processes and collaborate across disciplines, which results in engaged individuals on the team,” Naomi said.
“We focus on patient safety and confidentiality while working with our nurses to provide patient- and family-centered care by establishing connections between our patient families and UW Health’s incredible variety of resources,” Naomi said.

Nick Moorehead, certified nursing assistant

As Nick Moorehead worked his way up to a senior role in environmental services supporting the surgery team at University Hospital, he got a close-up look at the inner workings of what it takes to help nurses and other providers with patient care. “I am a person who loves to help others whenever I can,” Nick said.
His experience combined with his attitude made it an easier transition when Nick made the career move about a year ago to work as a nursing assistant (NA) after completing the internal UW Health program for nursing assistant certification.
Among his duties, Nick assists patients with personal hygiene, repositions them in their beds and takes their vital signs. Primarily working with orthopedic and medical patients at East Madison Hospital, he finds a way to connect with them, ensuring they are comfortable during their stay. Nick’s patients share their appreciation for his “can-do” attitude and his ability to brighten their day with his smile, even through the mask.
“I am motivated by knowing I can come into work to help different patients and their families through the tough times of being in the hospital,” Nick said.
Check out more stories featuring the great work of our nurses in the 2022 Nursing Annual Report (pdf).
Frontline focus on improvement
Within a large academic health system like UW Health, collaboration is an important element of our culture. It keeps the organization moving forward and allows staff and providers to share in both the work and rewards. When it comes to improvements, an identified gap or dissatisfier is followed by a plan for how to improve the issue. In these instances, frontline nurses are often the visionaries who ignite the change.
Improving post-hospital education for transplant patients
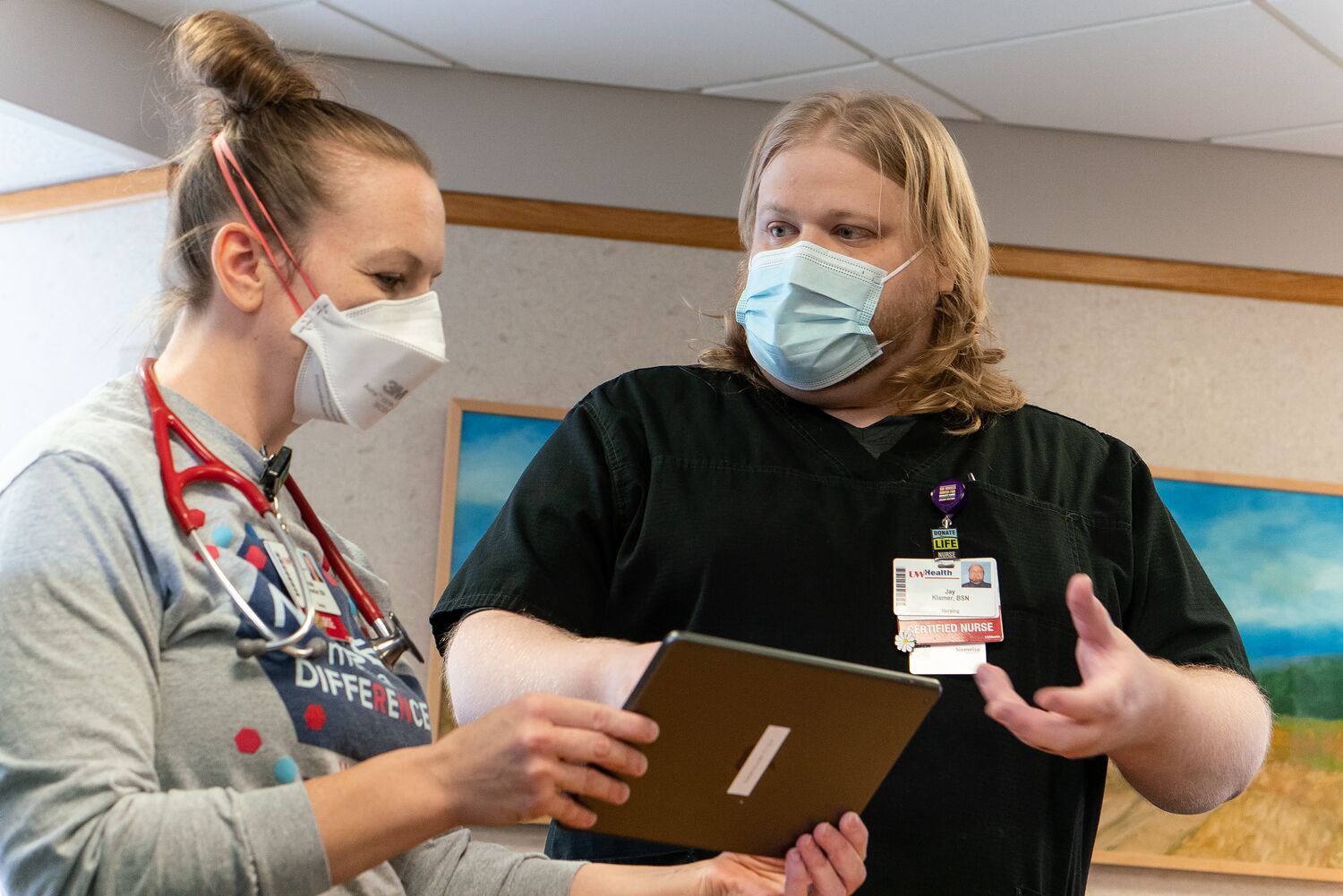
When Jay Klamer, BSN, RN, started working on the Transplant Unit at University Hospital, daily patient and family education sessions were held in the nearby family lounge.
“It was great because transplant patients and their support people would attend along with nurses and pharmacists,” Jay said. “The sessions were very useful because the patients and families could interact with the care team and ask questions.”
Unfortunately, that changed in early 2020 with the onset of COVID-19 pandemic. The transplant teams could no longer use the lounge, so they moved to nurse-to-family and nurse-to-patient models, which weren’t as effective.
“When there is one person instead of eight providing the education, it takes less time away from patient care. Providing all the education at discharge takes a lot more time and is very challenging for the person managing the discharge,” Jay said of the resulting strain on nurses. “It was equally difficult for patients who weren’t getting their post-hospital care education needs met because everyone was doing it differently.”
That’s when Jay knew there was a better way to help patients and his nursing colleagues.

The first attempt to fix the issue involved patients using iPads to attend a daily virtual class led by a clinical nurse specialist or nurse.
“Consistency was still a challenge and support people would often miss it due to COVID visitor restrictions,” Jay said. “So, I took a closer look at how much we were missing and wondered how we could fill in the gaps.”
Jay recalled that pharmacy had a similar issue and subsequently changed their class to a video format, which provided more viewing flexibility for patients. He realized this same approach would help transplant patients receive the education they needed, while greatly helping nurses from a time perspective.
Jay standardized the video content and engaged key colleagues, including clinical nurse specialists Gwen Klinkner, DNP, RN, BC-ADM, CDE; and Jess Viste, DNP, RN, ACNS-BC, CCTM.
“I could not have gotten this far without the help from Gwen and Jess,” Jay said, noting that Gwen ensured the language was at the appropriate medical literacy level and helped with scripting, while Jess provided the core educational content and reviewed everything for accuracy.
Although creating the videos has taken more time than Jay anticipated, he is excited to help patients and nurses once all videos are accessible via MyChart and uwhealth.org. “We have robust written versions of our materials, but there are limitations. Having this education available on video improves access for all patients and will help everyone in the long run.”
Pre-admission discharge planning is a win for patients

It’s safe to assume that no one wants to be hospitalized longer than necessary. Unfortunately, there are instances when patients are medically ready for discharge but unable to leave for an outlying reason, such as needing long-term care and a nursing home bed is not available. These are referred to as “avoidable days” and cause a ripple of dissatisfaction for patients ready for discharge and those in need of care. The cost also adds up.
Outcomes manager Katie Meicher, BSN, RN, identified an opportunity to address this preventable issue with improvements to case management workflows.

“It had been hypothesized that discharge planning before scheduled surgical admissions would provide several benefits,” Katie said. “It could reduce avoidable days as well as the number of patients turned away, while improving patient satisfaction, outcomes and hospital capacity issues,” Katie said.
To put things in motion, Katie conducted a test of change on a subset of vascular surgery patients who met the criteria of having a planned surgery. Prior to admission, they were called by a case manager for an initial interview to gather information pertinent to discharge planning, and to help set reasonable expectations for the length of stay and anticipated discharge needs. Case management was then able to start pre-admission discharge planning.
“The results were astonishing,” Katie remarked. “Not only did the six-month test of change reduce avoidable days by greater than 90%, we discovered an unintended benefit — there was more time to reprioritize patients who were urgently admitted but had at least 24 hours before going to the operating room.”
With the prioritization of those patients, the vascular surgery case manager was able to begin discharge planning pre-operatively, thereby reducing avoidable days in that population by greater than 90% as well. The estimated annual financial impact of this intervention was a reduction in cost of $245,813 with a projected reduction of over $3.1 million annually once scaled across surgical services.
“Follow-up survey data also revealed that the patient experience had been overwhelmingly positive regarding the reduction of avoidable days and improved patient communications,” Katie said. “With further reduction of avoidable days, we project that bed availability will increase, benefitting patients in need of quaternary care.”
Check out more stories featuring the great work of our nurses in the 2022 Nursing Annual Report (pdf).
Nursing informaticists tuRN ideas into action
In health care, innovation is key to keep pace with the ever-changing landscape. Health care systems must be increasingly nimble, have a steady influx of innovative ideas and most importantly, teams that can execute those ideas.
Enter our esteemed nursing informatics colleagues, otherwise known as the “wizards behind the curtain” who wield their expertise to turn those ideas into action and progress.

One of the first to integrate two unique systems
When nursing informaticists Jade Lee, Chelsey Langer and Sandy Vergenz were presented with an innovative idea from inpatient nursing staff, they saw a prime opportunity to improve patient safety and nursing satisfaction.
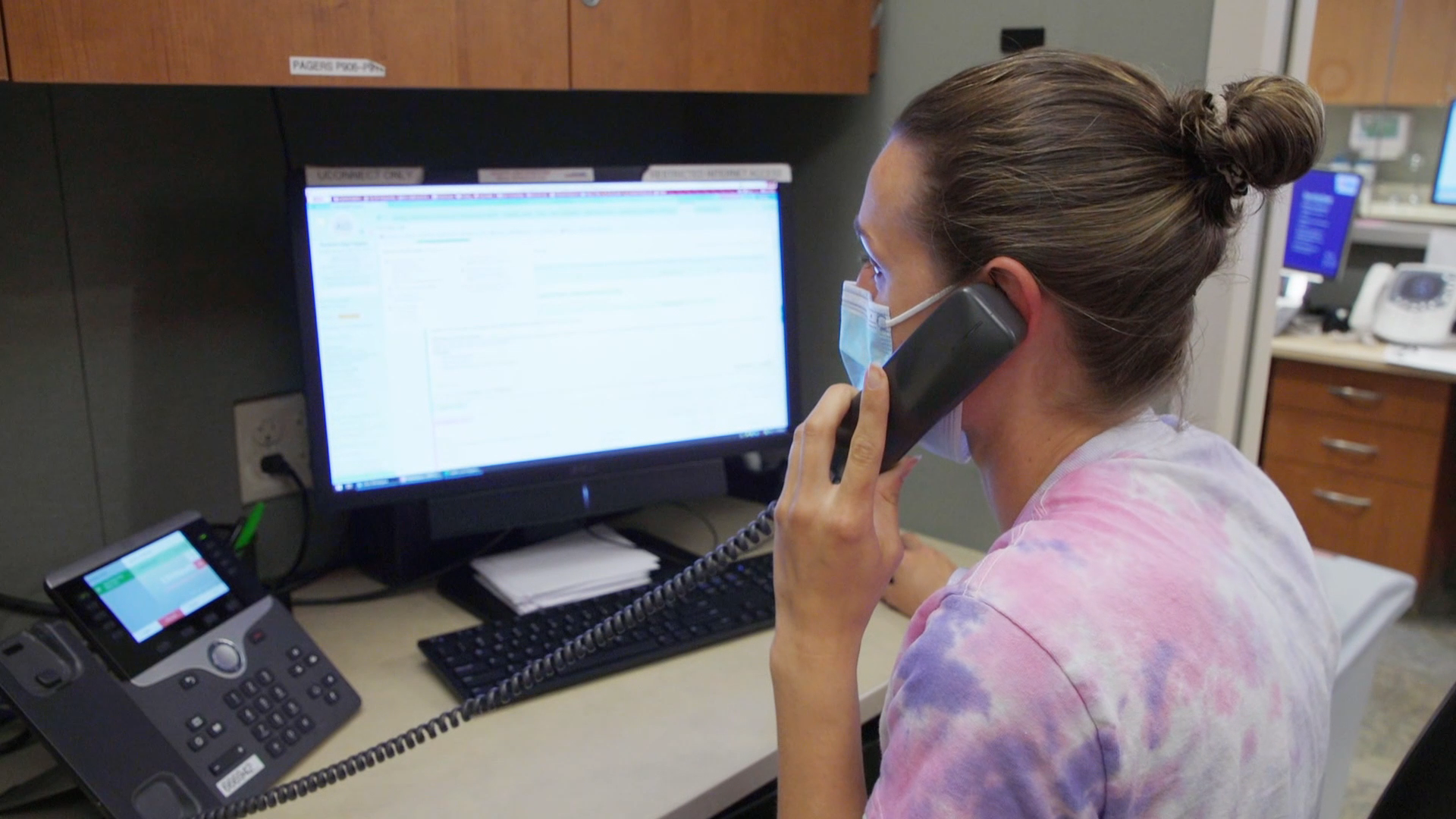
The idea pertained to the nurse call system (Responder 5) on inpatient units that provides dual alerts after a patient pushes a nurse call button: flashing lights outside the room that help nursing staff quickly identify the location and an alert/call to the unit desk that any care team member can answer to see if help is needed.
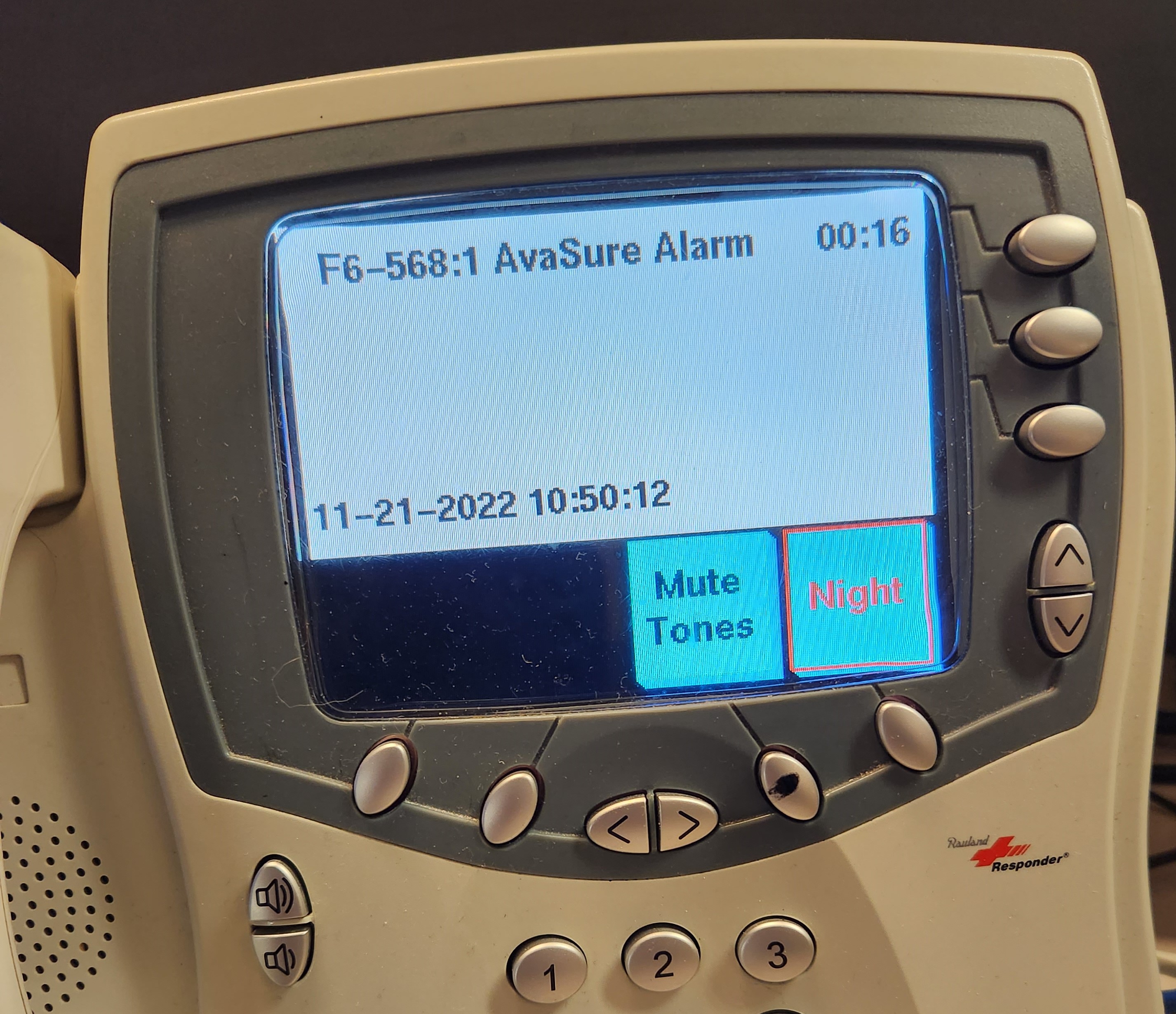
On units where constant observation cameras (AvaSure) are located inside patient rooms, the lack of visual alerts when an alarm was activated presented a challenge.
“Offsite video monitor technicians alert nurses to distress in those rooms by sounding an alarm and calling the unit desk,” Lee said. “The techs also were having to quickly multitask—speaking to the patient in the room while calling the unit desk — hindering nurse response time, which was exacerbated when there were multiple cameras in use on the unit.”
Langer added: “Based on what we knew about Responder 5 capabilities, we thought it made sense to align that function with the AvaSure cameras to help nursing staff quickly identify the patient room via a visual message on the nurse call console at the unit desk and initiating lights outside the patient room.”
When it was confirmed that the integration was possible, technicians from AvaSure and analysts from UW Health Unified Communications and the Health Link Inpatient teams were consulted for the Health Link (electronic medical record) build. It was a long and arduous process, but the nursing informaticists were a driving force and committed to making it happen.
Instead of moving to a pilot phase, the team “tested the heck out of it,” Lee said, adding that they went with a “big bang” approach and launched the integration on 23 of 31 units at University Hospital, American Family Children’s Hospital and East Madison Hospital. The remaining eight units will be integrated once they upgrade from Responder 4 to Responder 5.
“This was a wonderful collaboration that has improved patient safety and nurse efficiency by closing the gap on that critical window of time from when the observer sets off the alarm to when the nurse enters the room,” said Vergenz, who added that the icing on the cake was threefold. “Not only was UW Health one of the first health systems to make this type of integration possible, the reward of improving patient safety and nurse satisfaction is invaluable.”
Streamlining a process boosts patient and nurse satisfaction
Having a surgical procedure is stressful, so when Kerry Martin, MSN, RN, nurse manager, Thoracic Unit, University Hospital. saw an opportunity to improve the patient experience and streamline the workflow, she took action.
The issue? Patients coming out of surgery are understandably groggy and often want to be left alone. But a nurse needs to ask several questions to help care for them.
“Patients often ask ‘Don’t you have this in your computer already?’ or ‘Don’t you talk to each other?’ ” Kerry said. “Inpatient nurses know that having patients complete these questions at home before their procedure would be a much better process. It is just a matter of how that idea becomes a reality.”
Kerry submitted the suggestion — a pre-admission adult health assessment for surgical patients — to the UW Health Workforce Innovation Hub, an area on the organization’s intranet where staff can share innovative improvement ideas.
When Anne Mork, MS, MHCDS, RN, chief nursing officer of ambulatory services saw the submission, she immediately reached out to Linda Xiong, BSN, RN, interim director of nursing informatics, to make the idea a reality.
“We started with a test of change that involved care team leaders (CTLs) from University Hospital and East Madison Hospital, as well as first-day surgery RNs,” Linda said. “The goal was to have patients answer necessary questions in their optimal state, prior to surgery.” Three phases were involved:
- Phase 1: CTLs called patients at home who had pre-scheduled surgeries and would need hospitalization afterward. They passed along the information to the pre-op nurse to avoid repeating the process when the patient arrived on the day of their procedure.
- Phase 2: To optimize the pre-surgery downtime between nursing assessments and physician check-ins, patients in first-day surgery answered intake questions (on a hospital-provided iPad) that inpatient nurses previously asked after surgery.
- Phase 3: Admission questions were moved to MyChart in advance of surgery as a pre-admission questionnaire.
To gauge effectiveness, the nursing informatics team implemented a time study that revealed a time savings of 14-16 minutes per inpatient, while it saved pre-op nurses from asking 7-8 questions. Linda and her team rounded on those units following the launch to see how things were going.
“Nurses were so happy to hear about the project and that part of their admission process was done,” Linda said. “They were literally high-fiving us at the unit desk, which was incredibly rewarding for our team, knowing that we helped remove a burden for them.”
“Being part of this test of change has been exciting,” Kerry said. “It’s really fun to see when your idea goes to actual implementation and then expands to other units.”
Linda credits the success of this implementation to having great partners like Kerry and Ashley Bishop, RN, BSN, manager of perioperative services as well as the pre-op and inpatient nurses who were involved.
“Having some of the questions already answered allows the pre-op nurses to focus more on what matters most: Preparing and comforting our patients for surgery,” Ashley said.
“This was the type of project we love working on, proving that ideas are seen and nurses are being heard,” Linda said. “It’s an exciting time for our team, showing how we contribute to remarkable health care.”
Check out more stories featuring the great work of our nurses in the 2022 Nursing Annual Report (pdf).
Providing the tools for lifelong leaRNing

Even with the constant changes in health care, UW Health nurses are endlessly knowledgeable and incredibly skilled. But where do they go for the learning and professional development that allows them to be so infallible? This is where the Department of Nursing Professional Development comes in.
Nursing Professional Development includes more than 20 nursing education specialists who are responsible for clinical staff onboarding, professional development, new equipment, procedure and protocol training, and management of the prestigious Nurse Residency Program, which onboarded nearly 200 nurse residents this year.
Nursing education specialists work to ensure staff have the tools and education they need to be confident in their abilities to provide remarkable care and feel fulfilled working at UW Health.
“Mentorship and advocacy are the foundations of my practice as an educator,” said Molly Daniels, MSN, RN, CMSRN, nursing education specialist.
“We are champions for both the orientee and preceptor,” said Bianca Nelson, MSN, RN, CCRN, nursing education specialist. “Our job is to advocate for the nurse and tie education and professional development back to better patient outcomes.”

Tricia Ejzak, MSN, RN, CNOR, provided a closer look at her role as a nursing education specialist in the operating room:
Q: What does a typical day look like as a nursing education specialist?
A: Every day is different. As an NES in the operating room at East Madison Hospital, I am responsible for onboarding all new staff who will work in the OR. When someone starts, they spend their first week with me practicing skills and learning how to be safe in the space before moving on to work with a preceptor.
Since I work with the OR team, I monitor quality measures for surgical site infections and educate staff on opportunities for improvement. Another focus is continuing education. If there is a new procedure, new equipment or equipment that staff needs more experience with, I ensure they have the training they need. I also support staff with their professional goals and manage required trainings.
Q: It sounds like you also create process efficiency?
A: Absolutely! A new sports medicine surgeon started doing a procedure with a risk of significant blood loss. In those instances, we use a Fresenius Kabi Continuous Autotransfusion System to collect and clean blood for reinfusion. In the past, for every procedure, a trained technician from University Hospital had to travel to East Madison Hospital in case we needed to use the machine. Knowing the process could be more efficient, I coordinated training on the Fresenius Kabi Continuous Autotransfusion System for eight of our OR nurses. Now, we have trained staff at East Madison Hospital.
In addition, all the surgical nursing education specialists recently created a centralized OR orientation. We teach core content and utilize the UW Health Clinical Simulation Program facility for a more realistic training environment. With centralized orientation, we are more efficient and can now back each other up, when needed.
Q: How do you know what to focus on as an NES?
A: We get direct requests from staff members and feedback from surveys. I work closely with OR leadership who inform me of any practice and protocol changes.
Q: What is the best part of being an NES?
A: My job allows me to work with remarkable people in many different departments. I also enjoy being a part of the NPD team. Everyone is incredibly knowledgeable and supportive. It is tremendously fulfilling.
Nursing Education and Professional Development 2022 at UW Health
| Ambulatory: Clinical Staff Education Department | Inpatient: Nursing Professional Development Department | |
| Staff onboarded | Clinical staff: Registered nurses (RNs), medical assistants (MAs) and other clinical roles: 280 Non-clinical: 829 Online orientation: 734 employees Ambulatory nurse residents: 13 | Registered nurses: 524 Nursing assistants (NAs): 318 NAs hired through the NA Apprentice Program: 61 Age-friendly partner: 2 Student nursing assistants: 63 Nurse residents: 203 Nurse externs: 28 Personal safety observer: 1 Nursing care partners: 74 Anesthesia technicians: 2 Surgical technicians (STs): 7 ST travelers: 2 |
| Nurse resident cohorts | 2 with 432 hours of education provided, including 52 lectures from content experts and 15 skills sessions | 7 (increased from 6 to accommodate hiring more nurse residents sooner) |
| Staff trained | Retrained all primary care staff in COVID vaccine reconstitution and administration Conducted 75 N-95 trainings for specialty care clinics | Critical Care class: 111 Intravenous Ultrasound class: 81 Preceptor workshop: 202 Advanced Preceptor workshop: 28 Peripheral IV class and roadshow: 165 Nurse Resident (NR) IV skills: 147 Inpatient Trauma class: 80 Nursing assistant professional development: 68 Basic Arrhythmia class: 218 Continuous Renal Replacement Therapy Advanced User course: 54 Adult Stroke class: 35 Maternal mock code training to improve care and outcomes for pregnant patients: 56 RNs Non-violent crisis intervention (NVCI) Initial class: 54 NVCI Refresher class: 28 |
| Annual competencies/validation tools created for the staff-driven competency process | Comprehensive staff-driven competency packages for RNs: 9 Shifted medical assistant focus to CEU/educational opportunities | Competencies: 65 Validation Tools: 130 |
| Education requests completed | Completed Health Link (electronic medical record) Nurse Decision Support Tool rollout to primary care sites. Offered 180 hours of on-site triage support, 16 trainings and 12 Q&A sessions in addition to offering WebEx messaging RN support, Monday–Friday, 8 am–5 pm to nurses using the new tool. | In partnership with the Nursing Education Council, established Nursing Professional Development Days. |
| Other notable accomplishments | Competency management January 2022: Released competencies covering approximately 1,000 staff members as part of Annual Staff-driven Competency. Improved electronic process to make system more user-friendly for end user. Educators relieved managers of validation method checking and competency completion responsibilities. Evidence-based practice Held 24 Introduction to Triage and 7 Advanced Triage classes. Piloted one Nurse Extern cohort with 10 scheduled for 2023. | Perioperative nursing student shadow experience Spring 2022 collaboration with the University of Wisconsin-Madison School of Nursing to host nearly 50 Bachelor of Science in Nursing students for a perioperative shadow experience from First Day Surgery to intraoperative to Post-Anesthesia Care Unit. Revised Nurse Resident (NR) Orientation Added more hands-on skills and specific breakout sessions for pediatrics and surgical services. Goal was to provide NRs with more basic skills to help reduce the amount of teaching help needed from the nursing education specialist and reduce the preceptor workload on units. |
Check out more stories featuring the great work of our nurses in the 2022 Nursing Annual Report (pdf).
Evidence-based mentorship program

In 2015, when Kelly O’Connor, BSN, RN, CPN, started working at American Family Children’s Hospital, she noticed some personal challenges.
“It was really difficult to transition from being a student nurse to a new-to-practice nurse,” Kelly said. “As a student, you receive a lot of support. As a new nurse, there is a gap period after orientation with your preceptor until you feel confident on your own. You may feel alone and don’t yet have those authentic connections with other nurses for support.”
Kelly thought it was just her, until she started seeing those same challenges with other new nurses.
Knowing this may be more than a coincidence, Kelly did some research. It turns out, those common experiences of fear, disillusionment and overall stress felt by new-to-practice nurses are real and described as transition shock.
“I learned that transitioning into nursing is often traumatic, and new nurses may be fearful at work throughout their first year,” Kelly said.
She also found that there were distinct developmental stages that new-to-practice nurses went through, and that nurse mentorship programs helped ease those transitions.
With her research in mind, Kelly approached Élise Arsenault Knudsen, PhD, RN, ACNS-BC, nurse scientist who leads the Nursing Research and Evidence-Based Practice (EBP) Programs, about starting an EBP project focused on supporting new-to-practice nurses in her unit.
“To help retain new, bright nurses, we need to develop a culture that accepts and embraces them,” Kelly said. “A mentorship program is a first step in creating a positive loop: New nurses who are accepted, appreciated and guided will eventually offer the same acceptance, appreciation and guidance to new nurses who come after them.”
In 2022, Tessa Martin, BSN, RN, CPN, nurse manager of the Pediatric Medical/Surgical Unit where Kelly currently works, made the decision to include the mentorship program in the onboarding process for all new nurses on the unit. After the initial 14-week orientation where nurses are paired with a preceptor to learn the ropes, the new nurses are matched with an experienced frontline nurse mentor. For the next seven months, in addition to support on the unit, mentors and mentees meet outside of work for one hour each month to informally discuss any fears, concerns or highlights the new nurse wants to share.
Furthermore, Kelly created mentorship resources and worked with Tessa to distribute information about the program to staff and nurse residents.
“In addition to the mentor/mentee relationships, we created a visual management board in our conference room that staff can reference at any time,” Tessa said. “We also posted the new nurse development stages that Kelly identified through her research and have our mentor/mentee pairs printed on cards to show their progress through the stages.”
“The mentorship program has become incredibly successful. Our job is really hard, and this program helps acknowledge those feelings and supports new graduates through those evidence-based struggles.”

Check out more stories featuring the great work of our nurses in the 2022 Nursing Annual Report (pdf).
Supporting our communities, near and far
From orphanages and hospitals in Africa to breast cancer research and support for patients here at home, UW Health nurses are there for our communities near and far.
‘Mama Susan’s’ strong bonds in Africa
January 2023 marked the 20th year for Susan Gold, BSN, RN, ACRN, and her volunteering efforts with HIV/AIDS patients in Africa. In January, she brought the latest group, now totaling 122, of UW-Madison students who are interested in global health to Africa. They help teach the “Talking Health Out Loud” curriculum on sexuality and healthy relationships that Susan developed.

Susan is the only clinical nurse to have won a Fulbright Grant, a Washington Mandela Fellowship and a national Magnet Nurse of the Year Award. She said her Tanzanian patients have many questions about HIV treatments and are curious about the different treatments available in the United States.
“Being a nurse gives you credibility,” she said, “as does being trained in patient education in the UW Health HIV/AIDS Clinic.”
Susan retired from her full-time work in the UW Health HIV/AIDS Clinic but continues to work as a per-diem nurse. Her nursing achievements are more amazing considering she didn’t earn her nursing degree until the week she turned 40. She was busy raising three children and it took her more than five years to graduate, although she did graduate top in her class.
“I think being a UW Health nurse is an honor and being able to represent the UW School of Nursing all over the world is a big honor,” she said. “I so strongly believe in the Wisconsin Idea and that the education you get from the school could benefit the whole world. You have knowledge that can save lives everywhere.”
The African connection started when she and her husband, Tim, climbed Mount Kilimanjaro. “The guides knew I was a nurse and said, ‘Come back and help our people,’ ’’ she said. “And when I came down off that mountain, I knew I could do anything.”
Susan first started working with AIDS orphans in Kenya. As they lived into adulthood as HIV-positive people, she saw the need for the sexuality education curriculum she developed. Her work moved to Tanzania as the security situation in Kenya worsened.
Over the years, she’s watched proudly as the global health students she’s introduced to Africa have gone on to earn degrees and become nurses, physicians, physician assistants, therapists and public health professionals. She was even able to introduce some of her grown children and grandchildren to Tanzania, where she is known as “Mama Susan.”
All heart in Rwanda
A group of nurses on the Cardiothoracic Surgery and Transplant Unit also have a strong bond with Africa after traveling to Rwanda as part of Team Heart. This volunteer group was founded by a Boston nurse who visited Rwanda and found a hospital ward full of young people whose hearts had been damaged when untreated strep throat progressed to rheumatic fever and heart valve damage. The group has been going to Rwanda to perform heart surgery since 2008.
Recently, though, the focus has shifted to building sustainable cardiac care in Rwanda, and that is where the cardiothoracic nurses come in. Nurses Alexa Callahan, BSN, RN; Mikayla Kohls, BSN, RN; and Bella Penniston, BSN, RN, have all traveled to King Faisal Hospital in Kigali to teach their Rwandan colleagues the fine points of caring for patients following heart surgery. Bella said she did international nursing work in India as a student and was thrilled to have the chance to go to Africa.
“The biggest difference is how young the patients are,’’ Bella said, noting that she was caring for teenagers with heart issues in Kigali, compared with the retirement-aged patients more common in Madison. She also enjoys working with Team Heart members from as far away as Iceland and Australia, noting that despite their different backgrounds, “health care is a universal language.”

“Our role is to be mentors and to foster education for Rwandan nurses,’’ said Alexa, winner of a 2022 Nurse Excellence Award. “We’re teaching them the nuances of taking care of patients post cardiac surgery, and how to recognize the little signs that tell you if a patient is doing well or not.”
All the teaching is done at the bedside, and sometimes, the differences in resources are jarring. Alexa saw shoelaces being used to keep breathing tubes in place, and ventilator tubes being sterilized and reused. Rwandan nurses have to mix their own infusion medications.
“It’s very bare bones, with much fewer resources,’’ she said. “But the Rwandan nurses are so smart and so eager to learn. They are very passionate about cardiac care.”
Spreading cheer locally
Michelle Hornung, BSN, RN, uses her flair for beauty to help support breast cancer research at the UW Health Breast Center.
“Paying it forward always feels great,’’ said Michelle, who uses her Crazy Daisy Instagram feed to promote breast cancer awareness. A breast cancer survivor herself, Hornung was touched when her chemo clinic nurses gave her a “Nurses Inspire Nurses” T-shirt.
When she returned to work after treatment, Michelle bought the shirts for her fellow nurses on her unit. “This is our way of spreading cheer to other nurses, who are human first and nurses second,’’ she said. “We are family.”

Check out more stories featuring the great work of our nurses in the 2022 Nursing Annual Report (pdf).
Sharpening our nursing strategic focus

Finalizing our nursing strategic plan in 2022 was an exciting milestone: We solidified our six areas of strategic focus that we are proudly introducing below. These areas serve as the foundation for the work we’ve already started and the exciting work that will continue for the next three to five years. Our efforts are directly connected to the UW Health Nursing vision: To serve as remarkable and trusted national leaders in nursing — every day.
To effectively move our work forward, we identified and prioritized two of these areas to serve as our main pillars: “Promote a culture of well-being” and “Attract and retain a talented workforce.” The first addresses the importance of seeing our nurses as humans first, and nurses second, thereby providing them with the self-care resources they need to be at their best, personally and professionally. Additionally, we continue to implement innovative strategies to attract and retain the best and brightest nurses to help address the national shortage and alleviate the staffing strain on our nurses. These two pillars are vital to sustaining a healthy and high-functioning nursing workforce, and therefore, support all other areas of strategic focus and help drive all work forward.
Promote a culture of well-being
Nurses must prioritize their own well-being to provide exceptional care to our patients. We will develop tactics and strategies to positively influence the holistic well-being of nurses throughout UW Health by creating an inclusive culture that supports and optimizes their emotional and physical health throughout their careers.
Attract and retain a talented workforce
The global workforce shortage has stressed the nursing profession. We will use innovative approaches to recruit new nurses and retain a highly skilled nursing workforce.
Elevate nurse influence
The voices of individual nurses and the collective nursing workforce have significant influence on the care provided to UW Health patients. Through the continued empowerment of our nurses, their influence will be elevated to positively impact patient outcomes and organizational decisions while increasing respect within care teams.
Enhance professional development
The nursing profession is a journey of continuous growth and development. UW Health nursing will enhance professional development opportunities to help our nurses remain astute to advancements in science and practice.
Expand health literacy
Patients should feel they are partners with UW Health and nurses throughout their health care experiences. We are committed to improving the degree to which patients feel empowered to find, understand, and use information and services that help them make informed health-related decisions.
Influence nursing practice nationally
Nurses within a Magnet institution ask questions, advance the science of nursing and disseminate work broadly. UW Health nursing will optimize opportunities for nurses to fully live UW Health’s Nursing vision: To serve as remarkable and trusted national leaders in nursing — every day.
We look forward to working together — with nurses across UW Health — to continue advancing our professional nursing practice and strategic plan. Stay tuned for future updates on our progress and the details of this important work.
Rudy Jackson, Chief Nurse Executive
Nicole Kalscheur, Chief Nursing Officer, East Madison Hospital
Michele McClure, Chief Nursing Officer, University Hospital
Anne Mork, Chief Nursing Officer, Ambulatory and Nursing Care Services
Luke Sticht, Chief Nursing Officer, American Family Children’s Hospital
Becky Kohler, Chief Nursing Information Officer
Sarah Brzozowski, Director, Magnet and Nurse Excellence
Check out more stories featuring the great work of our nurses in the 2022 Nursing Annual Report (pdf).
Leading, supporting and partnering with RNs

The essence of a leader is to serve as a visionary while providing guidance, support and the tools employees need to thrive. That’s why the nursing leadership structure at UW Health is designed to provide RNs with local support while promoting a culture of accessibility to all nursing leaders and transparency in communication.
Working with RNs to address important issues
Through the UW Health Nursing Shared Governance Council structure, nursing leaders attend system-level council meetings to provide executive support to each council and help move work forward, whenever needed. Two prime examples from 2022 pertain to the ever-hot topic of staffing:
- Short- and long-term staffing solutions
At the peak of the RN staffing crisis, executive nursing leaders quickly launched an Internal Traveler Program to leverage talent from within the organization to fill shifts, with additional pay incentives. Although the program was successful in filling 90% of open shifts, it was a short-term solution due to the financial strain on the organization. To work toward a more sustainable solution, leaders engaged the Nurse Staffing and Operations Council and other direct care RNs to gain insight on what might work best.
“The RN input we received was extremely insightful and helped us arrive at a long-term solution,” said Rudy Jackson, chief nurse executive.
The result was a phased staffing plan involving four phases based on need (normal, urgent, critical or crisis), with relative incentive pay per phase and shorter shift-length options. While staffing issues still exist, leaders continue to work with nurses on ways to address them. - Advocating for nurses and all staff
When the Flexing Staff to Work Volumes Policy went into effect in 2019, it established a process for instances when employees were reassigned or required to take time off, with or without pay, when staffing adjustments were needed based on patient volume and/or department workload. At that time, there was no cap on the number of hours an employee could be “flexed down,” which was a huge dissatisfier. Through robust collaboration with the Staffing and Operations Council and Betsy Clough, chief human resources officer, Rudy was able to advocate for employees across the organization to reduce the number of hours any employee could be flexed annually from 208 to 60 per year. The updated policy went into effect in July 2022.
Support at every level: Defining nursing leader roles
Aniqueka Scott, MPH, BSN, RN, has always had an interest in learning more about different nursing leader roles. So, when she decided to pursue her Doctor of Nursing Practice (DNP) degree, she explored the various levels of leadership through a DNP in Systems Leadership and Innovation practicum.
“This was a unique opportunity for me to evaluate leadership at various levels, see how they differ and how they interact with, support and complement each other,” said Aniqueka, who works on the Family Practice and Forensics Unit at University Hospital.
Through contact with UW Health leaders in meetings, steering committees and workgroups, Aniqueka learned about the oversight responsibility for each role and how it supports nurses.
- Nurse manager: Unit leader who provides oversight for a unit’s nursing operations and transitional care
- Nursing director: Oversees nurse managers and provides operational oversight of multiple units/areas or provides guidance for a particular area such as infection control
- Leader through influence: Oversees departments that support nursing and influence nursing outcomes such as education, quality/safety/infection control and shared governance
- Chief nursing officer (CNO): Provides oversight of a designated facility or services, and the respective nursing or clinic operations directors
- Chief nurse executive: Oversees CNOs and leads strategic organizational changes, including nursing and other departments
Aniqueka recognized two common threads among UW Health leadership roles: A genuine sense of concern for RNs on the frontline and a commitment to serving as mentors. “Not only do these leaders want to share their knowledge, they care what nurses have to say and want to support their roles in any way possible.”

Cultivating professional growth
When Aniqueka and Josh Ernst, BSN, RN, pursued their DNP degrees, they experienced the leadership culture from a new lens.
“UW Health nurse leaders have provided me with substantial support throughout my doctorate studies,” said Josh, who serves as a clinical program coordinator for the Telestroke Program. “With this experience, I learned from various leaders within the organization, and I will take their advice with me wherever I go.”
In one of Josh’s practicums, Melanie Hankes, BSN, RN, nurse manager, UW Health East Madison Hospital Emergency Department, showed him how to overcome unique department challenges by coming up with creative and innovative solutions. “Teamwork is essential and expectations are high,” he continued. “There is always a sustained commitment to our patients, staff and the community. It is nothing short of inspiring.”
What stands out most for Aniqueka is having leaders who believe in her.
“They see my potential, and no one has ever made me feel I was reaching too high or dreaming too big,” she said. “I’ve been supported by every leader I’ve interacted with, confirming my decision to get my DNP.”
Aniqueka said she’s received the same advice from many leaders: Stay curious and keep asking questions. One takeaway came to light when she saw the work that went into establishing the Internal Discharge Lounge that was quickly operationalized by nurses and nursing leaders to help free up inpatient beds.
“I’ll never forget when Michele McClure (chief nursing officer for University Hospital) said, ‘Don’t let perfection get in the way of progress. We didn’t get it perfect, but we were off to a good start,’” Aniqueka said. “That realistic approach — acknowledging the need to evolve — really stuck with me.”
Another notable moment was seeing the humility of the leaders.
“They are down-to-earth and want to hear from frontline nurses to learn how best to support them,” Aniqueka said. “It’s all about teamwork and willingness to have conversations to try and make things better for everyone.”

Check out more stories featuring the great work of our nurses in the 2022 Nursing Annual Report (pdf).
