In health care, innovation is key to keep pace with the ever-changing landscape. Health care systems must be increasingly nimble, have a steady influx of innovative ideas and most importantly, teams that can execute those ideas.
Enter our esteemed nursing informatics colleagues, otherwise known as the “wizards behind the curtain” who wield their expertise to turn those ideas into action and progress.

One of the first to integrate two unique systems
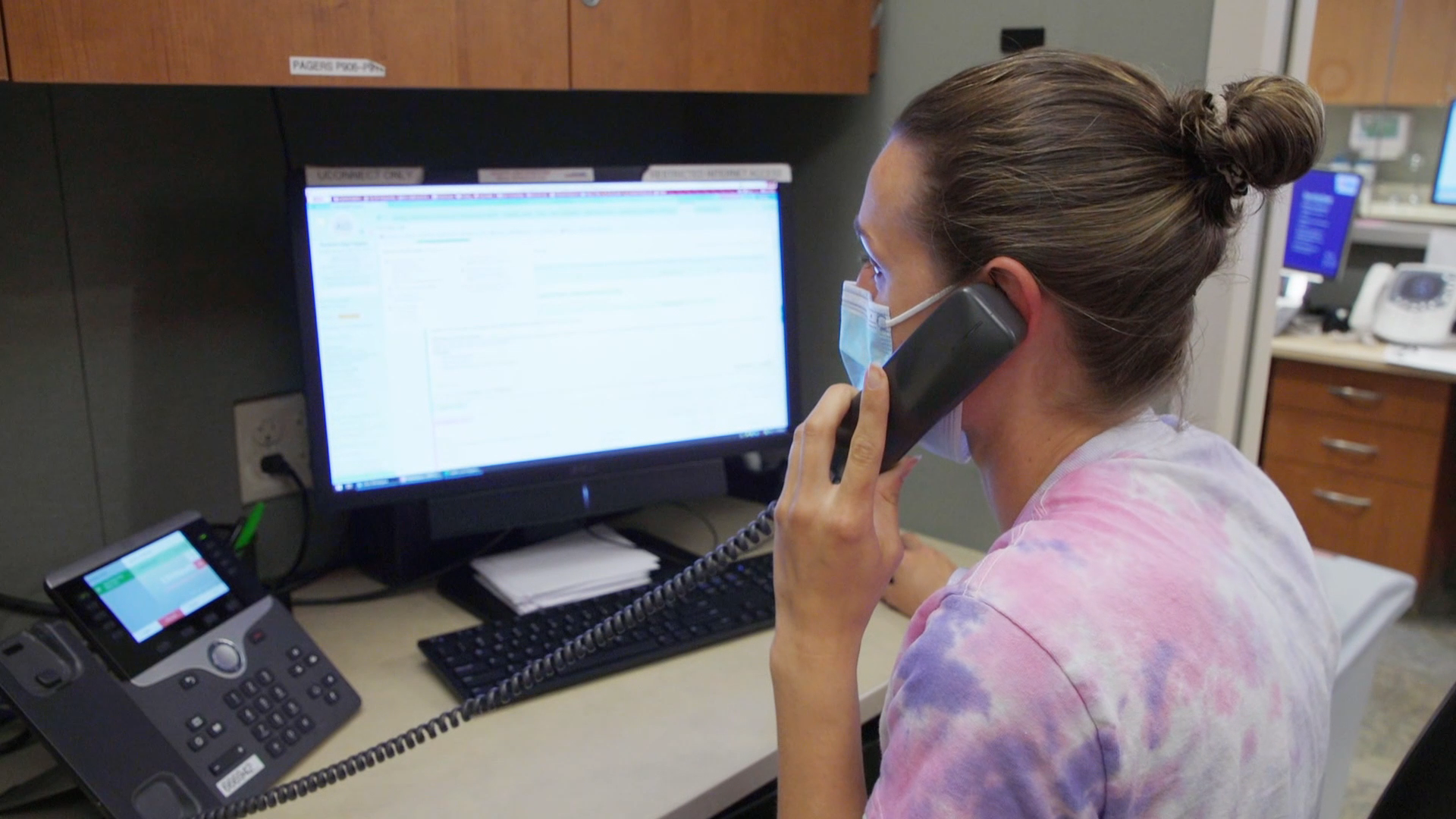
When nursing informaticists Jade Lee, Chelsey Langer and Sandy Vergenz were presented with an innovative idea from inpatient nursing staff, they saw a prime opportunity to improve patient safety and nursing satisfaction.
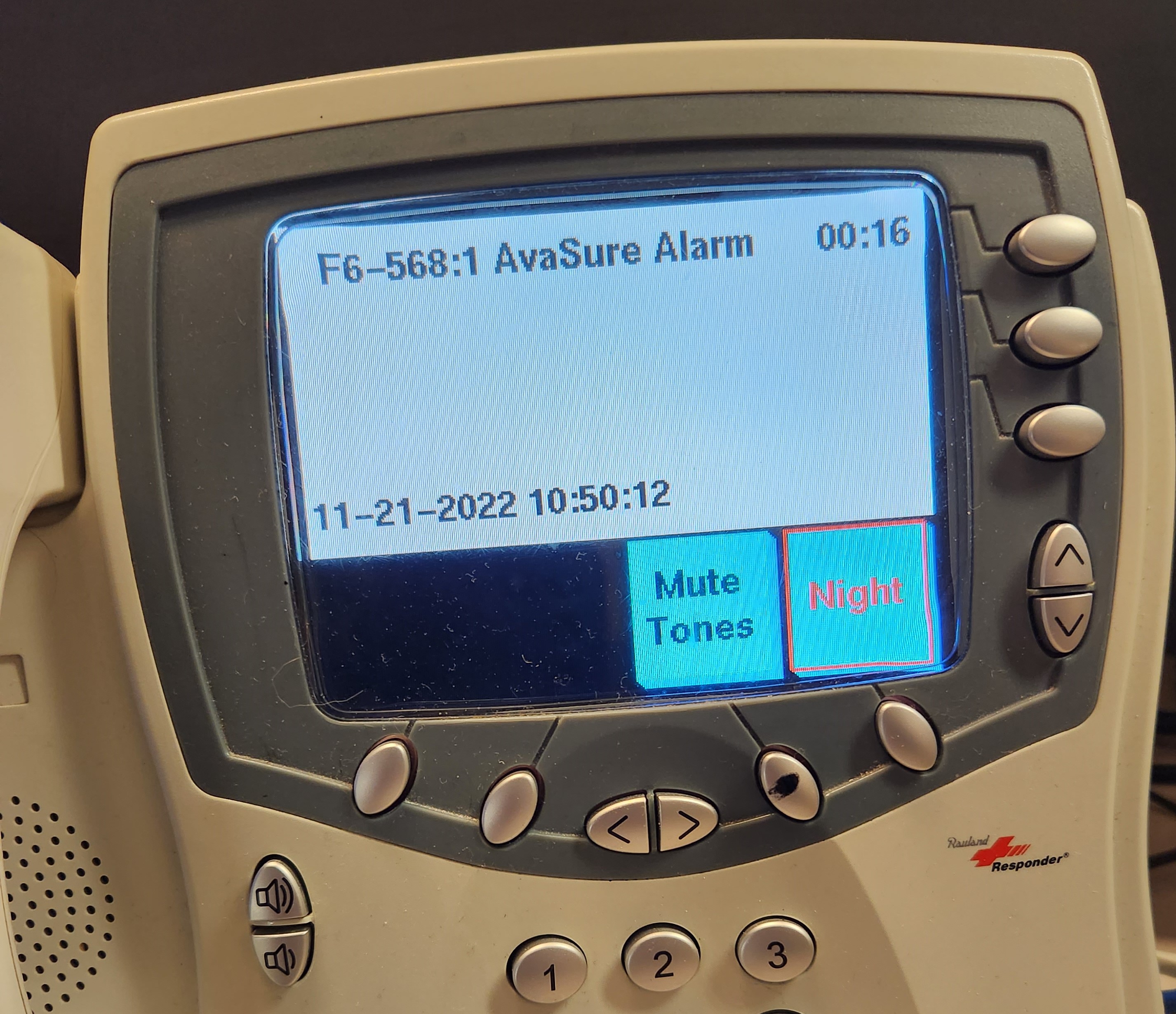
The idea pertained to the nurse call system (Responder 5) on inpatient units that provides dual alerts after a patient pushes a nurse call button: flashing lights outside the room that help nursing staff quickly identify the location and an alert/call to the unit desk that any care team member can answer to see if help is needed.
On units where constant observation cameras (AvaSure) are located inside patient rooms, the lack of visual alerts when an alarm was activated presented a challenge.
“Offsite video monitor technicians alert nurses to distress in those rooms by sounding an alarm and calling the unit desk,” Lee said. “The techs also were having to quickly multitask—speaking to the patient in the room while calling the unit desk — hindering nurse response time, which was exacerbated when there were multiple cameras in use on the unit.”
Langer added: “Based on what we knew about Responder 5 capabilities, we thought it made sense to align that function with the AvaSure cameras to help nursing staff quickly identify the patient room via a visual message on the nurse call console at the unit desk and initiating lights outside the patient room.”
When it was confirmed that the integration was possible, technicians from AvaSure and analysts from UW Health Unified Communications and the Health Link Inpatient teams were consulted for the Health Link (electronic medical record) build. It was a long and arduous process, but the nursing informaticists were a driving force and committed to making it happen.
Instead of moving to a pilot phase, the team “tested the heck out of it,” Lee said, adding that they went with a “big bang” approach and launched the integration on 23 of 31 units at University Hospital, American Family Children’s Hospital and East Madison Hospital. The remaining eight units will be integrated once they upgrade from Responder 4 to Responder 5.
“This was a wonderful collaboration that has improved patient safety and nurse efficiency by closing the gap on that critical window of time from when the observer sets off the alarm to when the nurse enters the room,” said Vergenz, who added that the icing on the cake was threefold. “Not only was UW Health one of the first health systems to make this type of integration possible, the reward of improving patient safety and nurse satisfaction is invaluable.”
Streamlining a process boosts patient and nurse satisfaction
Having a surgical procedure is stressful, so when Kerry Martin, MSN, RN, nurse manager, Thoracic Unit, University Hospital. saw an opportunity to improve the patient experience and streamline the workflow, she took action.
The issue? Patients coming out of surgery are understandably groggy and often want to be left alone. But a nurse needs to ask several questions to help care for them.
“Patients often ask ‘Don’t you have this in your computer already?’ or ‘Don’t you talk to each other?’ ” Kerry said. “Inpatient nurses know that having patients complete these questions at home before their procedure would be a much better process. It is just a matter of how that idea becomes a reality.”
Kerry submitted the suggestion — a pre-admission adult health assessment for surgical patients — to the UW Health Workforce Innovation Hub, an area on the organization’s intranet where staff can share innovative improvement ideas.
When Anne Mork, MS, MHCDS, RN, chief nursing officer of ambulatory services saw the submission, she immediately reached out to Linda Xiong, BSN, RN, interim director of nursing informatics, to make the idea a reality.
“We started with a test of change that involved care team leaders (CTLs) from University Hospital and East Madison Hospital, as well as first-day surgery RNs,” Linda said. “The goal was to have patients answer necessary questions in their optimal state, prior to surgery.” Three phases were involved:
- Phase 1: CTLs called patients at home who had pre-scheduled surgeries and would need hospitalization afterward. They passed along the information to the pre-op nurse to avoid repeating the process when the patient arrived on the day of their procedure.
- Phase 2: To optimize the pre-surgery downtime between nursing assessments and physician check-ins, patients in first-day surgery answered intake questions (on a hospital-provided iPad) that inpatient nurses previously asked after surgery.
- Phase 3: Admission questions were moved to MyChart in advance of surgery as a pre-admission questionnaire.
To gauge effectiveness, the nursing informatics team implemented a time study that revealed a time savings of 14-16 minutes per inpatient, while it saved pre-op nurses from asking 7-8 questions. Linda and her team rounded on those units following the launch to see how things were going.
“Nurses were so happy to hear about the project and that part of their admission process was done,” Linda said. “They were literally high-fiving us at the unit desk, which was incredibly rewarding for our team, knowing that we helped remove a burden for them.”
“Being part of this test of change has been exciting,” Kerry said. “It’s really fun to see when your idea goes to actual implementation and then expands to other units.”
Linda credits the success of this implementation to having great partners like Kerry and Ashley Bishop, RN, BSN, manager of perioperative services as well as the pre-op and inpatient nurses who were involved.
“Having some of the questions already answered allows the pre-op nurses to focus more on what matters most: Preparing and comforting our patients for surgery,” Ashley said.
“This was the type of project we love working on, proving that ideas are seen and nurses are being heard,” Linda said. “It’s an exciting time for our team, showing how we contribute to remarkable health care.”
Check out more stories featuring the great work of our nurses in the 2022 Nursing Annual Report (pdf).
