UW Health Employees Respond to National Crises
When we reflect on 2017 as a nation, it was undoubtedly a year with a continuous drumbeat of tragedy. From devastating hurricanes hitting Texas, Florida and Puerto Rico, to the mass shootings in Las Vegas and Texas, most Americans felt helpless as they watched news feeds and wondered what they could do from afar.
At UW Health, it didn’t take long for several staff members to rally and fly into action.
Hurricane Irma
This fierce tropical storm entered the Florida Keys and moved north, devastating most of the state. Once the extent of the damage was reported, Safety and Emergency Management staff for UW Health approached senior executives with an idea to assemble a team to help contribute to the relief efforts in the south.
It didn’t take long for the idea to get approved and after discussing the needs, it was determined that a team comprised of Registered Nurses would be ideal for providing any necessary care to victims and helping with other volunteer efforts.
Within a couple of days, 75 UW Health RNs indicated they were ready and willing to make the trek.
Due to the overwhelming response, a selection process was implemented based on how many RNs UW Health could realistically send to Florida – factoring in schedules and patient care needs. The resulting UW Health team included six nurses from ambulatory, education, emergency services and inpatient areas, including: Donna Clift-Prew, BSN, RN; Holly Hatcher, RN, Jennifer Kooiman Mohr, MSN, RN-BC; Josue Maldonado, BSN, RN; Chadd Siebers, BSN, RN; and Michele McClure, MSN, RN.
When the team departed in September, they arrived in Naples, Fla., and traveled to one of four Medical Special Needs Shelters (MSNS).
The shelters initially housed close to 1,800 victims, but by the time the UW Health team arrived, the number of victims had been reduced to two. Rather than providing patient care, the UW Health team helped with demobilization of the shelter, which consisted of cots and supplies for more than 1,000 people.
The UW Health team joined several other nurses from across the US and were then dispatched to Tallahassee. The warehouse they worked in had sent out more than 10,000 ready-to-eat meals within the first few of days following the hurricane.
“It was my honor and privilege to be selected as one of six nurses to represent UW Health,” said Holly Hatcher, RN. “I absolutely believe in the power of giving back and we all learned so much on this trip – being flexible in a disaster recovery situation, emergency/disaster management processes, and more significantly – the importance of teamwork. I am so thankful for my managers’ support of the relief mission and for the opportunity to participate as part of the UW Health team. It was an amazing experience that I would gladly sign up for again.”
More Irma and Maria Missions
In addition to the Strike Team’s efforts, another UW Health nurse who is part of the Wisconsin National Disaster Medical Assistance Team (DMAT) through the Health and Human Services department experienced two back-to-back deployments.
Patty Scanlin, RN, NREMT-P, nurse care team leader for emergency services at UW Health at The American Center, also serves as the chief nursing officer for Wisconsin 1 DMAT. She joined 33 other members who were deployed to Hudson, Fla., along with other DMATs across the country.
“As soon as we arrived in Florida, we started providing patient care,” says Scanlin. “We had been up 36 hours. After that, we started working 12-hour shifts.”
In addition to helping care for 270 patients with often limited supplies and resources, some TLC was often needed for four-legged creatures, as well.
“The shelters stated that only service animals were to be allowed, but how do you keep hurricane victims and their very confused and anxious pets apart?” Scanlin asked. “We ended up allowing pets to be with their owners on the cots – there were more than 70. It was one simple act and a major stressor we could help remove for all of them – just by letting them be together.”
Scanlin recalls two instances where she and another team member helped care for pets.
“One anxious Labrador literally scratched the end of his nose from being frantic,” Scanlin said. “Another, older dog had an accident in his kennel so we gave him a bath.”
In addition to managing the furry friends amidst the chaos of patient care, Scanlin said there were more unexpected stressors that they had to contend with as well.
“DEA agents took us to our first shelter where there were also police and the National Guard. They were there to make sure everyone was safe,” Scanlin said. “The agents and police were all very vigilant and fortunately, I felt extremely safe. None of us needed to worry about these things on top of the hurricane destruction and victims in need of medical attention.”
Another unexpected concern that arose was when they realized that one particular hospice patient was close to death.
“One thing we didn’t set up for was where to place deceased bodies,” Scanlin said. “Fortunately, one of the members of our team was part of D-MORT (Disaster Mortuary Response Teams). He was able to find a room that had a locked door and would be designated as the on-site morgue. Thankfully, we never had to use it.”
Scanlin spent 11 days in Florida, returned home for two weeks and was deployed again for 16 days to Puerto Rico to assist with Hurricane Maria victims. Notification of each deployment came last minute, which Scanlin says is fairly common – often learning about them at night – and having to get on a flight the next day.
“I always have a bag ready to go,” she says. “At work, I feel guilty for leaving on such short notice, knowing that my coworkers and manager are burdened with my work. But I couldn’t have a more supportive team. I vividly recall telling my supervisor, Bridgett Schaeffer, that I would be willing to move to a staff nurse position if that would be better for everyone. Bridgett just looked at me and said, ‘No way – I support you 100 percent!’ – which was really nice to hear.”
Another comforting aspect Scanlin has appreciated throughout her mission work is knowing that her mental health and that of every DMAT member, is always supported.
“Each of us is followed up with by a mental health professional after every deployment, to make sure our re-entry into life and work back home is going well,” Scanlin said. “We have also formed amazing friendships among our teams, so it’s nice to know we can connect on Facebook anytime … and send each other silly Snapchats on occasion.”
Las Vegas Shooting
Just when the country thought it had witnessed more than enough destruction among storms and fires, an unimaginable tragedy took place in Las Vegas.
Seeing the numbers of victims that resulted from the mass shooting, one nurse at UW Health thought there might be a way to support the health professionals who were working round the clock to try and save lives.
“People who go into healthcare tend to put others first and their own needs on the back burner,” states Shelli Horne, BSN, RN, surgical services nurse at UW Health at The American Center. “Seeing what was taking place in Las Vegas, we knew those hospital workers were working long hours and days, and we thought sending food — as simple as it sounds — would be one way to offer support.”
Horne and two colleagues put out a call for donations to the rest of the UW Health at The American Center team and within two hours, they raised an impressive $1,700 for University Hospital in Las Vegas.
“We sent 51 pizzas to the Level One hospital the first day and then the next day we sent subs to two other area hospitals,” stated Horne. “We also donated $440 to the victim relief fund.”
Shortly thereafter, Horne said the disaster coordinator at the Level One hospital called to thank them for their efforts and let them know how much the pizzas were appreciated.
“It was the least we could do,” says Horne. “And comforting to know our efforts helped in some small way.”
View Channel 3000’s coverage of this story
Local Needs
Amid the national tragedies, a few UW Health staff members remained mindful of responding to ongoing community efforts, such as the fight against hunger and domestic abuse.
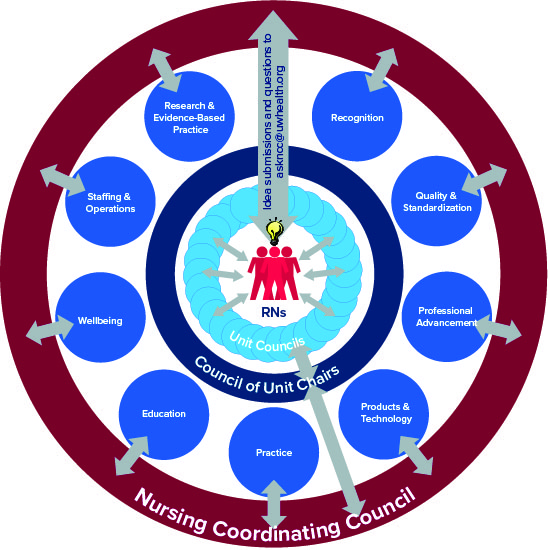
“Our Inpatient Operating Room (OR) RN Unit Council wanted to raise awareness about hunger issues in the community we serve every day,” stated Sara Booth, BSN, RN, inpatient OR nurse.
On Sept. 14, one of the local Madison news stations, WMTV NBC-15, challenged the city to post pictures of people wearing orange, to #Orange4SHFB on its Facebook page. For every picture posted, several local businesses committed to donating 23 meals per picture to the Second Harvest Food Bank.
“I thought it was a fun way for us to make a difference and I was thrilled to see that 27 of our operating room colleagues posted pictures,” stated Booth, who helped spread the word about the TV station’s challenge. “It was so fulfilling to know that those simple photographs resulted in 702 meals to Second Harvest!”
And the inpatient OR didn’t stop there.
In an effort to create camaraderie in the workplace and support two local organizations, Booth stated that the Inpatient OR RN Unit Council hosted a food and materials drive called “Fill the Box, Feed a Soul.” As a result of the drive, the council voted on supporting two organizations located in Dane County: Middleton Outreach Ministry (MOM) – one of the largest food banks in the county; and the Domestic Abuse Intervention Services (DAIS) – whose mission is to empower those affected by domestic violence and advocate for social change through support, education and outreach.
“From Sept. 23 through Oct. 1, we divided our OR staff into 10 teams, and food and clothing items were collected for donation throughout the week,” states Booth. “At the end of the week, we weighed the donations from each team and determined first and second place winners to receive a pizza and ice cream party, respectively (through funds raised by the OR staff).”
After each team’s donations were weighed, the total amount of donations to MOM and DAIS totaled more than 600 pounds.
“We are so thankful for and proud of our colleagues who coordinated and contributed to local and national relief efforts,” stated Beth Houlahan, DNP, RN, CENP, Senior Vice President, Chief Nurse Executive. “Their efforts speak volumes about the type of staff we have at UW Health … remarkable.”